Join us on a captivating journey as we explore the intricate workings of the heart. In this comprehensive guide, we dive into the basics of cardiac anatomy and physiology, unraveling the awe-inspiring mechanisms that keep this vital organ ticking. From understanding the heart's chambers and valves to exploring its electrical system, we provide a clear and accessible overview to enhance your knowledge.
Unveiling the heart's
fascinating beat and pump
Average heart rate
60-100bpm
Normal blood pressure
<120/80
Average blood pumped
5-6.0 litres/min
Our heart is usually the size of our fist and weighs around 250grams
The essentials that keep us beating
In this section, we embark on a fascinating exploration of the heart's remarkable anatomy and function. Delve into the intricacies of the heart's four chambers—the atria and ventricles—and gain a deeper understanding of how they work together in perfect harmony. Discover the major blood vessels that carry life-giving oxygenated blood from the heart to every corner of the body, and learn about the crucial role they play in sustaining our health.
Moreover, we delve into the captivating world of the heart's electrical system, uncovering the intricate web of impulses that orchestrate its rhythmic beat. Gain insights into the pacemaker cells, electrical pathways, and regulatory mechanisms that ensure the heart functions reliably and efficiently.
The cardiac muscle
The heart muscle, or myocardium, is a specialized type of muscle that makes up the walls of the heart. The myocardium is responsible for contracting and relaxing to pump blood throughout the body.
The heart muscle is unique in that it is constantly active, even when the body is at rest. The myocardium is able to generate its own electrical impulses, which stimulate the contraction of the heart muscle.
The heart muscle is made up of specialized cells called cardiomyocytes, which are connected by intercalated discs. These discs allow for the rapid transmission of electrical signals between cells, allowing the heart to contract in a coordinated and efficient manner.
The heart muscle has two important functions known as systolic and diastolic function. Systolic function refers to the ability of the heart to contract and pump blood out to the body. During systole, the myocardium contracts, and the heart chambers empty out the blood they were holding, sending it out to the lungs and body. Diastolic function, on the other hand, refers to the ability of the heart to relax and fill up with blood. During diastole, the myocardium relaxes, and the heart chambers refill with blood from the veins.
The coordination of these two functions is essential for the proper functioning of the heart and circulation of blood throughout the body. Systolic and diastolic function can be affected by a variety of factors, including damage to the heart muscle, high blood pressure, and certain medical conditions. Measuring and monitoring these functions can be important in diagnosing and managing heart conditions.
The heart valves
The heart's four valves play a critical role in ensuring that blood flows smoothly through the heart, from the right atrium to the right ventricle, and from the left atrium to the left ventricle.
The tricuspid valve is located between the right atrium and the right ventricle. It has three cusps or flaps that open and close to control blood flow. When the heart muscle contracts, the tricuspid valve opens, allowing blood to flow from the right atrium to the right ventricle. When the heart relaxes, the tricuspid valve closes, preventing blood from flowing back into the atrium.
The pulmonary valve is located between the right ventricle and the pulmonary artery, which carries blood to the lungs. It is also composed of three cusps and works in a similar fashion to the tricuspid valve. When the right ventricle contracts, the pulmonary valve opens, allowing blood to flow into the pulmonary artery and on to the lungs. When the heart relaxes, the pulmonary valve closes, preventing blood from flowing back into the right ventricle.
The mitral valve, also known as the bicuspid valve, is located between the left atrium and left ventricle. It is named after the resemblance of its two cusps to a bishop's mitre or hat. The mitral valve opens when the left atrium contracts, allowing blood to flow into the left ventricle. When the ventricle contracts, the mitral valve closes, preventing blood from flowing back into the atrium.
Finally, the aortic valve is located between the left ventricle and the aorta, the largest artery in the body. The aortic valve has three cusps and works in a similar way to the pulmonary valve. When the left ventricle contracts, the aortic valve opens, allowing blood to flow into the aorta and out to the rest of the body. When the heart relaxes, the aortic valve closes, preventing blood from flowing back into the ventricle.
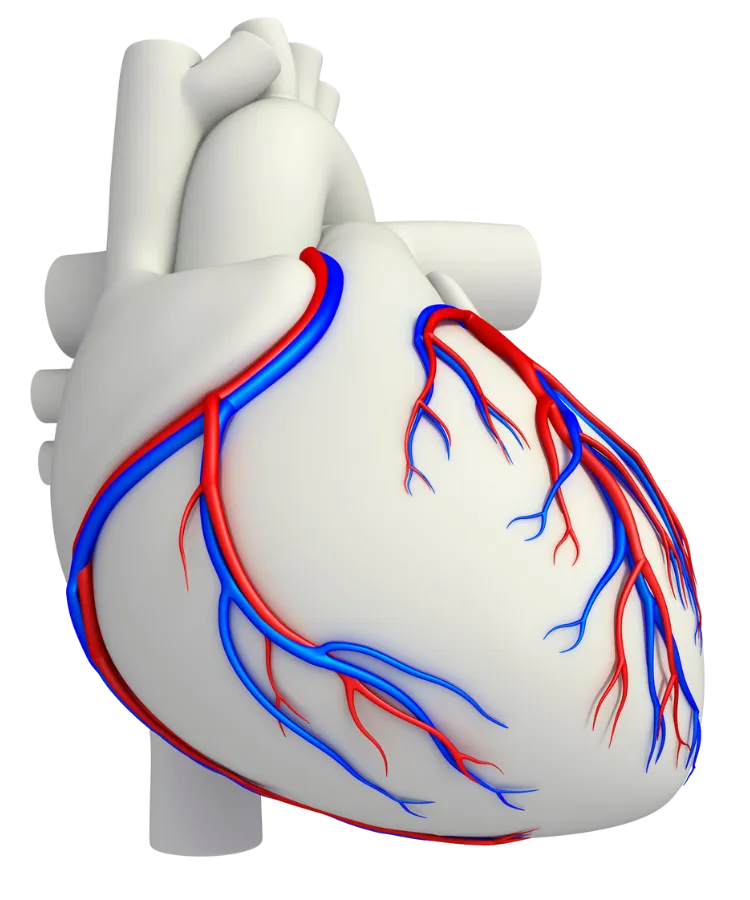
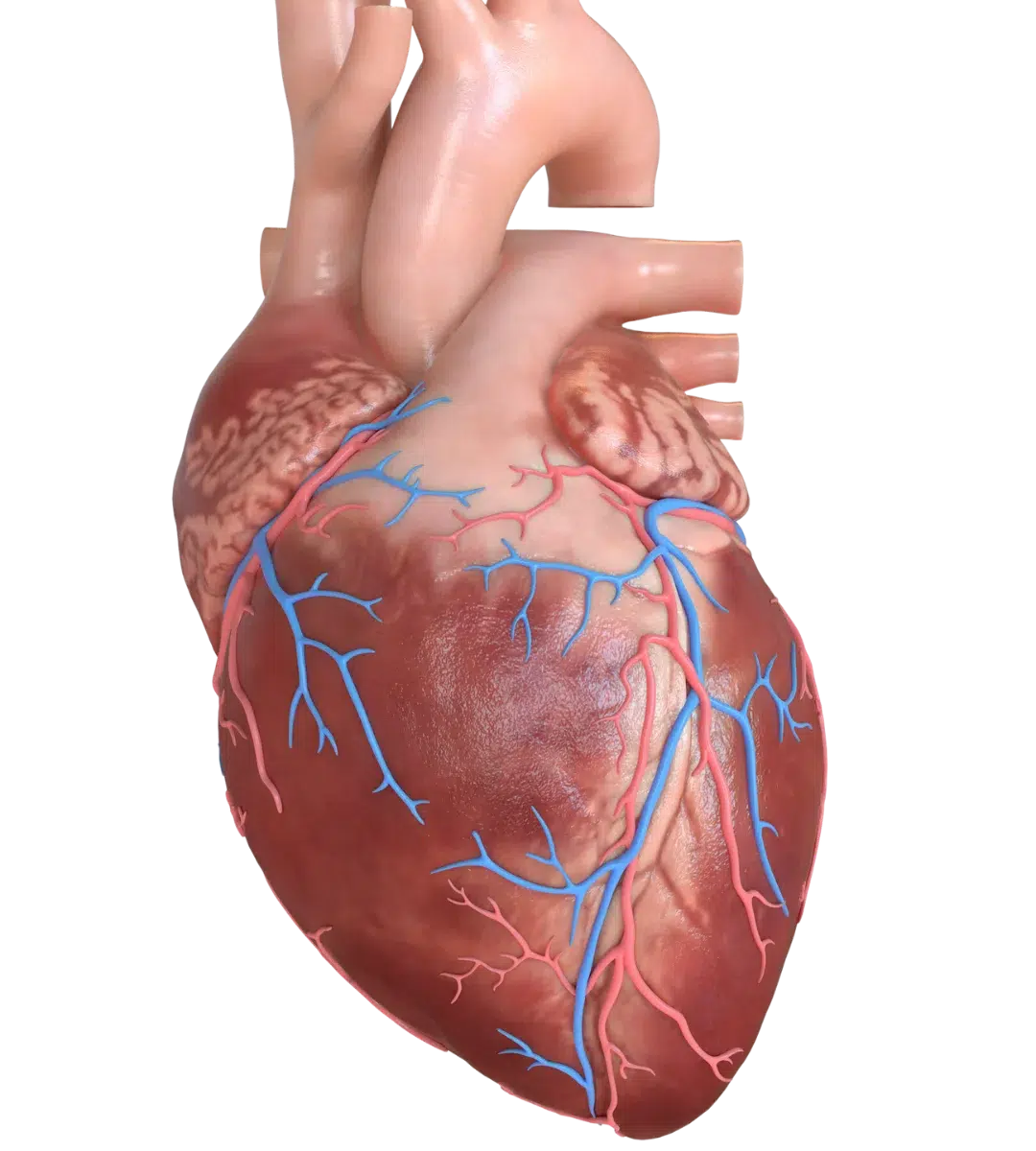
The coronary arteries
The coronary arteries are blood vessels that supply the heart with oxygen and nutrients. These arteries are essential for the proper functioning of the heart, and any blockages or damage to them can lead to important health complications.
There are two main coronary arteries: the left coronary artery and the right coronary artery. The left coronary artery branches off into two smaller arteries, the left anterior descending artery and the circumflex artery. These arteries supply blood to the left side of the heart, including the left ventricle, which is responsible for pumping oxygen-rich blood to the rest of the body. The left anterior descending artery (LAD) is one of the two main branches of the left coronary artery and is considered the largest of the coronary arteries. Its size and location make it a critical artery for the functioning of the heart, supplying blood to the front and left side of the heart, including the left ventricle, which is responsible for pumping blood to the rest of the body.
The right coronary artery supplies blood to the right side of the heart, including the right ventricle, which pumps blood to the lungs to be oxygenated. The coronary arteries are located on the surface of the heart and are encased in a layer of fat and connective tissue, known as the epicardium.
Blockages in the coronary arteries can lead to a condition known as coronary artery disease (CAD), which is a leading cause of heart attacks. CAD occurs when plaque builds up in the walls of the coronary arteries, causing them to narrow and reducing blood flow to the heart.
The conduction system
The human heart is an incredible organ that works tirelessly to keep us alive. It is responsible for pumping blood to the rest of the body, supplying vital nutrients and oxygen to our cells. One of the key components of the heart's function is its conduction system.
The conduction system is a network of specialized cells that control the rhythmic beating of the heart. These cells are located within the heart's walls and are responsible for generating and coordinating electrical impulses that regulate the heartbeat.
The conduction system begins in the sinoatrial (SA) node, which is located in the upper-right chamber of the heart, known as the right atrium. The SA node is often referred to as the "natural pacemaker" of the heart because it initiates the electrical impulses that signal the heart to beat.
From the SA node, the electrical impulses travel through a series of specialized cells, known as the atrioventricular (AV) node. The AV node is located in the lower-right chamber of the heart, known as the right ventricle. The AV node serves as a gatekeeper, slowing down the electrical impulses and allowing the atria to fully contract before the ventricles are activated.
After passing through the AV node, the electrical impulses travel down a bundle of specialized fibers, known as the bundle of His, which divides into two branches, one for each ventricle. These branches then further divide into Purkinje fibers, which spread throughout the ventricles, triggering the coordinated contraction of the heart's muscle fibers.
The conduction system of the heart ensures that the heartbeat remains synchronized and rhythmic, allowing for efficient pumping of blood throughout the body.
stay in the know
Stay informed about cardiovascular health with our newsletter. Get the latest insights, valuable tips, expert advice, and educational content delivered straight to your inbox.
