Coronary Artery Bypass Grafting (CABG) is a vital surgical intervention frequently conducted worldwide. It represents a substantial option that raises concerns and uncertainties owing to its significant impact. Nevertheless, amidst these hesitations, the potential advantages of CABG, particularly for certain patients, become evident. In specific cases, this procedure underscores its superiority over alternative approaches like stents, highlighting its ability to improve cardiac health outcomes. In addressing coronary artery disease, CABG emerges as a significant tool, offering a well-established pathway to tackle its intricacies.
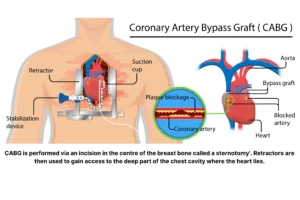
Coronary artery bypass surgery, also known as CABG (coronary artery bypass grafting and pronounced “cabbage”), constitutes a frequent surgical approach for treating coronary artery disease (CAD). The procedure involves rerouting blood flow around a blocked or narrowed section of a coronary artery, restoring blood flow to the heart muscle, and reducing the risk of heart attack.
Dr. Rene Favaloro, an Argentinean surgeon, performed the inaugural CABG surgery in 1960. Since then, this procedure has experienced notable advancements, remaining one of the most efficacious treatments for CAD.
 An example of an operating theater where CABG is performed
An example of an operating theater where CABG is performed
Indications for Coronary Artery Bypass Surgery
CABG surgery is usually advised for patients with severe coronary artery disease unresponsive to other treatments like lifestyle changes, medication, or angioplasty. It’s also considered for those with specific heart valve issues or congenital heart defects.
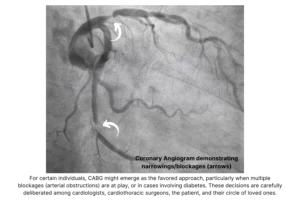
Healthcare providers frequently advise the surgery for patients with severe narrowing or blockage in the left main heart artery and/or multiple heart arteries affected by disease. When coronary angioplasty, a procedure utilizing a balloon or stent to expand the artery, cannot address a blocked heart artery, bypass surgery might emerge as the optimal choice. Moreover, if previous attempts at angioplasty or stenting prove unsuccessful, such as in cases where an artery narrows again following treatment, the procedure could be suggested.
Techniques for Coronary Artery Bypass Surgery
CABG surgery offers the option of being performed with or without a cardiopulmonary bypass machine, often called a heart-lung machine. This machine temporarily takes on the roles of the heart and lungs during surgery, enabling the surgeon to halt the heart briefly while grafts are attached. This approach is termed “on-pump” CABG surgery.
A less invasive alternative known as “off-pump” CABG surgery has emerged recently. This technique avoids the need to stop the heart and eliminates the requirement for the cardiopulmonary bypass machine. Off-pump CABG surgery may link to fewer complications, including bleeding, infections, and cognitive decline.
Benefits of Coronary Artery Bypass Surgery vs. Stenting
Although stenting is less invasive than CABG surgery, specific scenarios may favor the latter as a superior choice. For instance, patients dealing with left main or triple-vessel coronary artery disease often witness better outcomes with CABG surgery, leading to reduced complications. Moreover, for patients with diabetes who face increased risk with stenting, CABG surgery could emerge as the preferred alternative.
CABG surgery may also be indicated in patients with coexisting valve conditions that require surgery. CABG surgery can be performed simultaneously as valve repair or replacement surgery.
Risks of CABG
Like all surgeries, CABG has inherent risks, which is crucial. The risks vary depending on your pre-surgery health. Deciding on surgery involves balancing risks and benefits; it shows that professionals believe the risk to your well-being is greater without it. Below is a list of key risks common to surgeries, not just CABG. Your unique situation determines the likelihood of these complications. Discussing these risks with your healthcare provider is vital for an informed decision on CABG. It’s important to note that this list provides a broad overview and is not comprehensive:
-
Bleeding: Surgical procedures can lead to bleeding at the incision site and internally.
-
Infection: Infections can develop at the surgical site, in the chest, or other body parts.
-
Kidney Problems: Changes in blood flow during surgery can affect kidney function, leading to temporary or persistent kidney issues.
-
Irregular Heart Rhythms (Arrhythmias): Surgery can cause the heart’s electrical system to be disrupted, resulting in irregular heartbeats.
-
Stroke: There’s a risk of a stroke occurring due to factors such as blood clot formation or reduced blood flow to the brain.
-
Breathing Issues: Some patients may experience difficulties with breathing, mainly if the surgery affects lung function.
-
Memory Loss and Cognitive Difficulties: Temporary memory loss or cognitive challenges might arise, though they usually resolve over time.
-
Graft Failure: The grafts used in the surgery might not function as intended, leading to inadequate blood flow.
-
Wound Complications: The incision site can develop issues like poor healing, infection, or scarring.
-
Fluid Buildup: Fluid accumulation around the heart or lungs can occur, affecting breathing and cardiac function.
-
Blood Clots: Blood clots can form in the legs (deep vein thrombosis) or travel to the lungs (pulmonary embolism).
-
Heart Attack: Though rare, a heart attack can occur during or after the procedure due to changes in blood flow.
-
Reaction to Anesthesia: Some patients might experience adverse reactions to anesthesia or other medications.
-
Cardiac Tamponade: Fluid accumulation around the heart can compress it, reducing cardiac function.
-
Gastrointestinal Issues: Digestive problems, such as nausea, vomiting, or reduced appetite, can arise.
-
Emotional and Psychological Effects: Some patients might experience anxiety, depression, or emotional adjustment issues post-surgery.
Patients harboring pre-existing conditions such as stroke, leg artery blockages, chronic obstructive pulmonary disease (COPD), diabetes, obstructive sleep apnea, or kidney ailments could face elevated risks of complications. In emergency procedures, the odds of complications might be further escalated. Initiating a discussion with your Cardiologist and Cardiothoracic Surgeon regarding potential risks before coronary artery bypass surgery is essential.
The Heart Team
Multidisciplinary heart team discussions are pivotal in shaping the landscape of medical decisions, especially regarding procedures like CABG. With the growing emphasis on comprehensive patient care, these collaborative discussions involve diverse medical experts, each contributing their specialized insights. This approach ensures that all facets of a patient’s health condition are thoroughly evaluated, and potential treatment options are weighed meticulously. The collective knowledge and perspectives of cardiologists, surgeons, anesthesiologists, and other specialists foster a holistic understanding of the patient’s needs and risks. As multidisciplinary heart team discussions increase in the context of CABG, patients can be confident that their treatment plan results from a thorough, well-informed consensus aiming to optimize outcomes and enhance overall well-being.
The Surgical Procedure: What to expect
When undergoing coronary artery bypass surgery, you will be admitted to a hospital and cared for by a team of heart specialists, including cardiovascular surgeons and cardiologists.

Surgeons at work in an operating theater performing coronary artery bypass surgery
Before the surgery, you will be assessed by an anesthetist who specializes in administering anesthesia to patients during surgery. They are responsible for assessing the patient’s medical history and condition, determining the appropriate type and amount of anesthesia, monitoring the patient’s vital signs during the procedure, and managing any complications that may arise during or after anesthesia. You will be given a sedative through an intravenous line (IV) to help you relax.
Once in the operating room, you will be put under general anesthesia using a combination of medicines administered through the IV and a face mask. A breathing tube will be inserted into your mouth and attached to a ventilator, which will breathe for you during and immediately after the surgery. During the surgery, a heart-lung machine will keep blood and oxygen flowing throughout your body.
The surgery typically lasts 3 to 6 hours, depending on the number of arteries that are blocked.
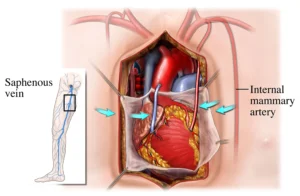
The surgeon will make an extended cut down the center of your chest (known as a sternotomy), spread open your ribcage, and stop your heart temporarily with medication. The surgeon will then remove a healthy section of the blood vessel, often from inside the chest wall (the mammary artery), the forearm (the radial artery), or the lower leg (saphenous vein graft), to create a new pathway for blood flow around the blockage. More than one graft may be used, depending on the extent of the blockage.
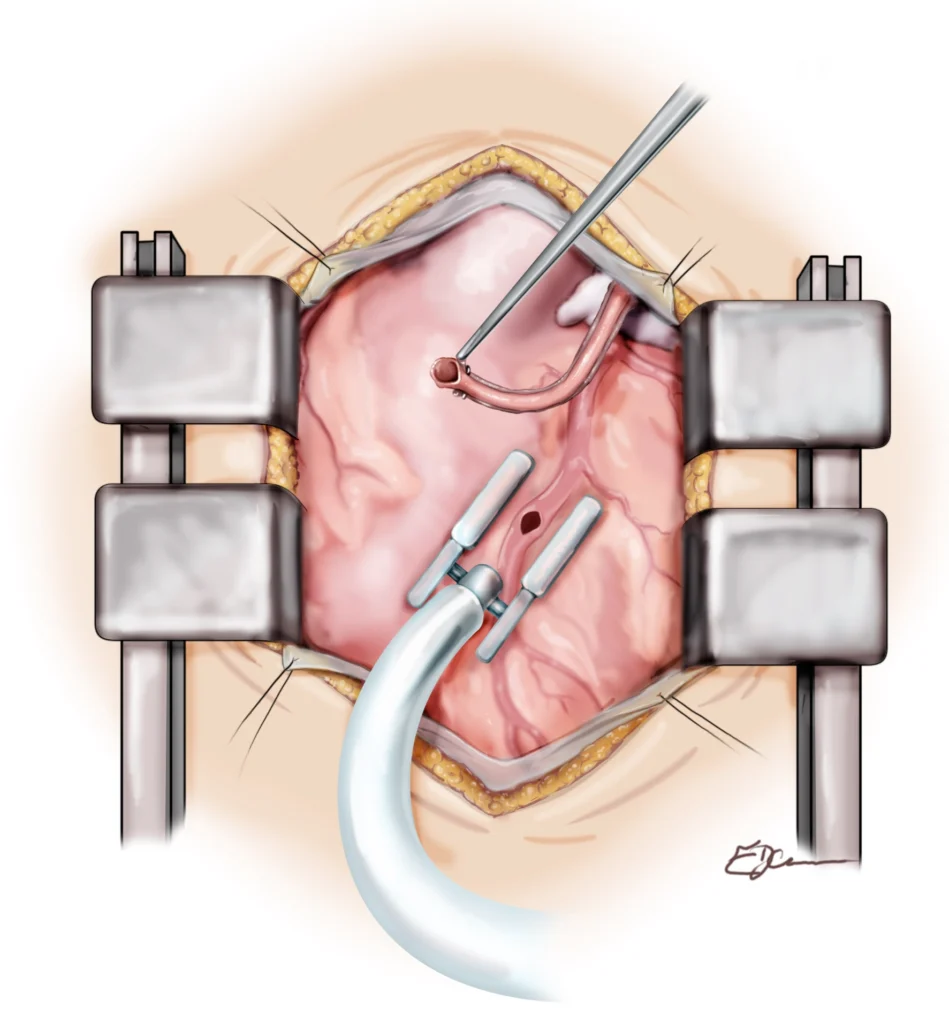 Off-pump Bypass with the artery stabilized
Off-pump Bypass with the artery stabilized
The Bypass Machine
In the realm of CABG, an often critical instrument steps into the spotlight – the bypass machine, often referred to as the heart-lung machine. This sophisticated apparatus assumes control over vital circulatory functions during surgery, temporarily relieving your heart of its pumping and oxygenating responsibilities. As the surgeon meticulously constructs new pathways to navigate obstructed arteries, the bypass machine circulates oxygen-rich blood throughout your body, ensuring oxygen delivery to your organs and tissues. An example of this is shown below. It is worth noting the heart-lung machine’s orchestration falls under the skilled purview of a perfusionist, adding another layer of expertise to the surgical ensemble.
The perfusionist controls the heart-lung machine in the operating theater.
In some cases, there’s a twist in the plan – it’s the off-pump CABG approach. Although the heart-lung machine usually plays a key role, off-pump CABG changes things. This time around, the surgery happens without the machine stepping in. Instead, the surgeon skillfully manages the operation while your heart pumps blood. The decision to use either method depends on your health and the surgeon’s know-how. This choice highlights the blend of traditional and innovative approaches. It’s important to remember that both methods have their strengths and considerations.
The heart-lung machine in action
Recovery from Coronary Artery Bypass Surgery
After CABG surgery, patients typically spend several days in the hospital, with the average hospital stay lasting around 5-7 days. During this time, patients will be monitored closely for signs of complications, such as bleeding, infection, or heart rhythm disturbances.
After CABG, your body needs time to heal. Here are some key points to keep in mind during your recovery:
Breathing Tube
After surgery, you will generally have a breathing tube in your throat to help you breathe. This tube is usually removed within 24 hours of surgery, but in some cases, it may stay in longer. You’ll need to be able to breathe on your own before the tube can be removed.
Hospital Stay
After surgery, you’ll spend at least one night in the intensive care unit (ICU). Your length of stay in the ICU will depend on how well you’re recovering. You can expect to be in hospital for about a week, give or take a few days, depending on how your recovery progresses.
Heart Rhythm and Breathing Checks
Your healthcare team will monitor your heart rhythm and breathing closely after surgery. You may have a telemetry monitor device that records your heart rate and rhythm. You will likely also have a few drain tubes placed within the chest to allow fluids to drain post-operatively, together with temporary pacing wires used as a precaution in the recovery phase for a few days in case the heartbeat slows down too much. You’ll also have frequent temperature checks. Your team will check your breathing to ensure your lungs are clear and you get enough oxygen.
Medicines
After CABG surgery, you’ll receive medications to manage pain and prevent complications. You may receive aspirin, blood thinners, and medications to lower blood pressure, heart rate, and cholesterol. It’s essential to take all medications as prescribed. Some of the commonly used medicines for those with established coronary artery disease can be found on our dedicated coronary artery disease page online by clicking here.
Cardiac Rehabilitation
Cardiac rehabilitation is an integral part of recovery after CABG surgery. This program includes supervised exercise, education, and counseling. You’ll begin cardiac rehab while in the hospital and then continue the program as an outpatient. Cardiac rehab aims to improve your heart health and reduce your risk of future heart problems.

An example of a cardiac rehabilitation session. Here, you will learn all about your cardiac condition and obtain helpful information to assist in speeding up your recovery following surgery and ways to reduce any further risks or complications for the future.
Watch for Complications
After surgery, it’s essential to watch for signs of complications. Contact your healthcare provider if you experience fever, rapid heart rate, new or worsening pain around your chest wound, a change in skin color around your chest wound, or bleeding or discharge from your chest wound. It’s essential to follow all post-operative instructions your healthcare team provides to ensure a smooth recovery.
After leaving the hospital, patients will continue to recover at home, gradually increasing their activity level over several weeks. Most patients can return to normal activities within 6-12 weeks of surgery, although this can vary depending on the individual and the extent of the surgery. You must work with your healthcare professional to optimize cardiovascular risk factors to ensure long-lasting results following surgery. Remember, these include stopping smoking, controlling blood pressure and diabetes, and working on strategies to reduce cholesterol plaque build-up.
The sternotomy incision is the surgeon’s cut to access the heart and perform the operation. The sternum is securely fastened with stitches, wires, or specific metallic plates to fix closed the sternum (breast bone). Smaller incisions are also made to allow passage of chest drain tubes and temporary pacemaker wires that support the heart early in the recovery period. Such drain tubes and wires are usually removed in a matter of a few days after the operation.
Graft Selection
Arterial Grafts:
Arterial grafts are taken from inside the chest wall, usually the left internal mammary artery (LIMA). LIMA grafts are the most commonly used arterial grafts in CABG surgery, while the right internal mammary artery (RIMA) and the radial artery, located in the forearm, are frequently also used. Arterial grafts are preferred over venous grafts because they are less prone to getting blocked and usually last longer. Arterial grafts can last up to 20 years, and the risk of them getting blocked over time is less than 10%.
Venous Grafts:
Venous grafts are taken from the saphenous vein in the leg. Venous grafts are used when there are no other suitable arteries to use as a graft. Venous grafts have a shorter lifespan than arterial grafts and can become blocked over time. Approximately 10-20% of venous grafts become blocked within the first year after CABG surgery and about half become blocked within ten years.
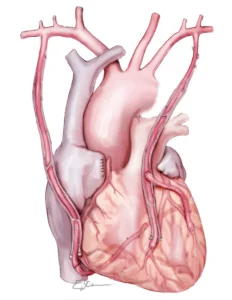
Example of multiple arterial grafts used for CABG
Comparison of Arterial and Venous Grafts
Arterial grafts are preferred over venous grafts because they are less prone to getting blocked and usually last longer. However, arterial grafts are more difficult to harvest, and not all patients are good candidates for this type of graft. In contrast, venous grafts are easier to harvest and can be used in most patients, but they have a higher risk of getting blocked over time.
 This surgical illustration depicts the post-operative condition of a coronary artery bypass procedure with a saphenous vein graft and an internal mammary-coronary artery anastomosis. The heart, pericardium, saphenous vein graft, internal mammary artery, and all the great vessels, including the aorta, superior vena cava, and pulmonary artery, are viewed through a midline thoracic incision.
This surgical illustration depicts the post-operative condition of a coronary artery bypass procedure with a saphenous vein graft and an internal mammary-coronary artery anastomosis. The heart, pericardium, saphenous vein graft, internal mammary artery, and all the great vessels, including the aorta, superior vena cava, and pulmonary artery, are viewed through a midline thoracic incision.
In summary, the lifespan of CABG grafts varies depending on whether they are arterial or venous. Arterial grafts have a longer lifespan and are less prone to getting blocked than venous grafts. The graft choice depends on individual patient characteristics and the surgeon’s preferences.
Single, double, triple, quadruple bypass surgery
The terminology of single, double, triple, and quadruple bypass surgeries reflects the extent of cardiovascular disease that necessitates revascularization. During these procedures, the surgeon aims to address blockages and impaired blood flow within the coronary arteries. A single bypass entails creating a new pathway for blood flow around one blockage, while double, triple, and quadruple bypasses address two, three, or four blockages. The decision on the number of bypasses needed reflects the severity and location of the arterial disease. Surgeons prioritize revascularizing crucial heart regions to optimize blood supply and support its proper function. This approach aims to enhance cardiac performance and overall patient well-being, aligning with addressing the most vital areas of concern during bypass surgery.
Learn more about the blood flow of our heart on our dedicated Heart Works page here.
The importance of the left anterior descending (LAD) artery
The left anterior descending artery (LAD) is important in guiding decisions for CABG surgeries. Renowned for its vital role in supplying a substantial portion of the heart with blood and oxygen, the condition of the LAD plays a crucial role in the decision-making process. Surgeons meticulously evaluate the health of the LAD as a pivotal prognostic factor, influencing the choice to proceed with CABG. Addressing any obstructions in this artery becomes paramount, highlighting the surgical approach’s emphasis on critical areas.
While the role of the LAD in influencing CABG decisions is noteworthy, it’s essential to recognize that surgery can still offer benefits in cases where the LAD isn’t directly implicated. Such scenarios are typically considered when symptoms persist despite other treatments or when additional coronary artery disease must be addressed alongside procedures to treat diseased heart valves.
Closure of the chest
In CABG, the chest closure plays a crucial role in ensuring the stability and healing of the surgical site. Traditionally, the closure involved using sternal wires threaded through the sternum to hold it together during recovery. This method has been successfully employed for many years and has proven effective in achieving chest stability. However, advancements in surgical techniques have introduced a contemporary approach utilizing sternal plate systems.
With the evolution of medical technology, sternal plate systems have gained popularity in recent years. These systems consist of rigid plates made of biocompatible materials, such as titanium or stainless steel, affixed to the sternum using specialized screws. The plates provide enhanced stability, allowing for better alignment and reduced motion of the sternum during the healing process.
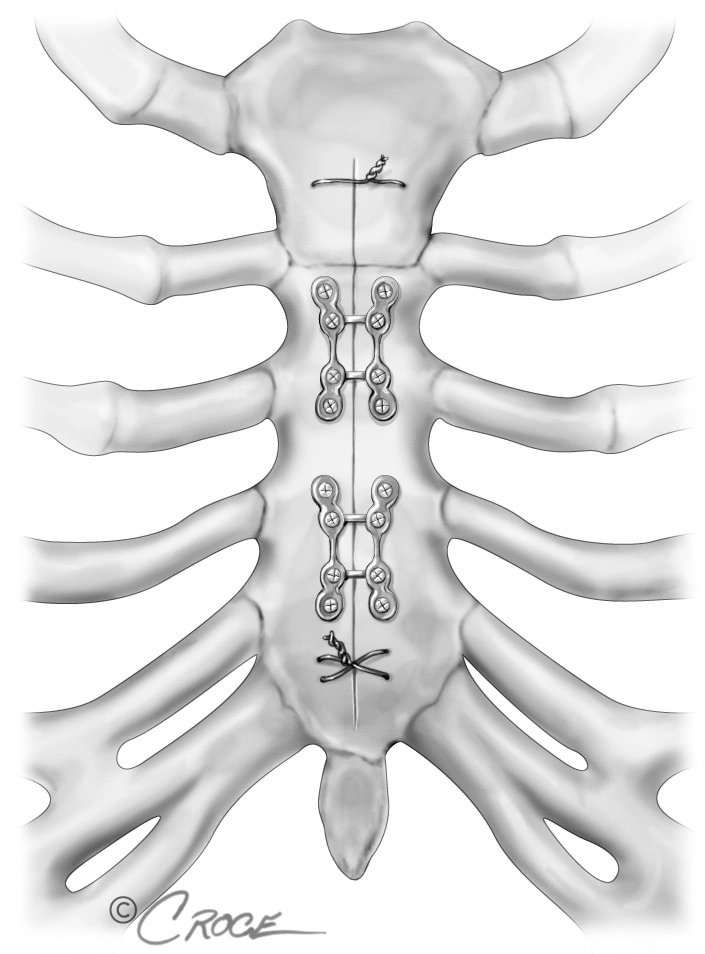
The chest plate system used to hold closed the sternum (breast bone) immediately following bypass surgery
Embarking on the journey of surgery can understandably evoke initial concern due to its significance, yet it’s reassuring to note that the remarkable benefits, both in terms of symptom relief and long-term prognosis, often become evident shortly after the procedure.
Conclusion
In conclusion, CABG surgery is a highly effective treatment for severe coronary artery disease, and it has undergone significant advances since its development over 60 years ago. While stenting is a less invasive option for some patients, CABG surgery may be better in certain situations, such as in patients with left main or triple-vessel disease, diabetes, or coexisting valve conditions. Recovery from CABG surgery can take several weeks, but most patients can return to normal activities and enjoy improved heart health after surgery.