As a cardiologist, I see daily how cardiovascular diseases affect people and their loved ones. It constantly reminds us to understand and address cardiovascular risk factors. While age and genetics are beyond our control, several lifestyle factors significantly contribute to heart disease risk. In this article, I’ll offer insights into these factors and their impact on cardiovascular disease risk. Understanding them helps us make informed choices and prioritize heart health.
Age
Age is an important cardiovascular risk factor that deserves attention and understanding. As we grow older, the risk of developing heart disease increases. This is due to various factors, including the natural aging process, cumulative exposure to other risk factors over time, and age-related changes in the body.
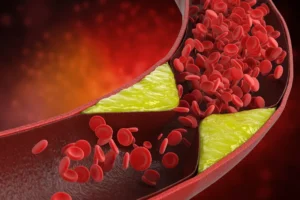
The arteries tend to become less flexible and more rigid with age, making them more prone to plaque buildup, a condition known as atherosclerosis. Additionally, age-related changes in the heart muscle and valves can affect its function and increase the risk of heart-related complications.
It is essential to note that age is a non-modifiable risk factor, but it does not mean that heart disease is inevitable as we age. By adopting a healthy lifestyle, managing other risk factors such as high blood pressure and high cholesterol, and seeking regular medical check-ups, we can mitigate the impact of age on our cardiovascular health. Remember, it’s never too late to start making positive changes that can positively influence our cardiovascular well-being.
Gender
Gender significantly affects cardiac risk, with distinctions in susceptibility and manifestations. Men have a higher prevalence of heart disease at younger ages, primarily coronary artery disease leading to early heart events like heart attacks and angina.
In contrast, women face unique challenges. Estrogen offers protection before menopause, but after, the risk rises due to estrogen decline. Pregnancy-related issues can also raise future cardiovascular risks.
Symptoms vary by gender, with men experiencing classic chest pain while women may have subtler signs like fatigue, shortness of breath, nausea, or back pain. This disparity underscores the need for gender-specific diagnostic approaches to prevent underdiagnosis or delays.
Family History
Genetics and family history are key factors in cardiovascular disease development. Family history raises risk due to shared genes and environmental factors. Certain genetic variants can also affect lipid metabolism, blood pressure, and inflammation, increasing susceptibility. Lifestyle choices like a healthy diet, exercise, and avoiding tobacco can lower risk, even with a genetic predisposition.
When we mention having a family history of cardiovascular disease, I’m not referring to Grandma, who might have had a heart attack in her 80s. Instead, we pay closer attention to early-onset events like heart attacks or strokes, particularly in immediate family members under 60. Even more significant is if these events occurred in relatives at a much younger age.
Additionally, genetic factors can contribute to an increased likelihood of conditions like high cholesterol and high blood pressure. These genetic predispositions serve as valuable indicators that help guide us in remaining vigilant about monitoring and managing these aspects of our health. We can proactively address and mitigate potential cholesterol and blood pressure risks by acknowledging these genetic influences.
High blood pressure
High blood pressure, or hypertension, is a leading risk factor for cardiovascular disease. It puts extra strain on the heart and blood vessels, increasing the risk of heart attack, stroke, and other serious conditions. The good news is that, if necessary, hypertension can be managed through lifestyle changes and medication. Some lifestyle changes that can help lower blood pressure include reducing salt intake, increasing physical activity, maintaining a healthy weight, and limiting alcohol consumption.
Blood pressure is measured in millimeters of mercury (mmHg) and is expressed as two values: systolic pressure over diastolic pressure. The systolic pressure represents the force exerted on the artery walls when the heart contracts, while the diastolic pressure reflects the pressure when the heart is at rest between beats.

A 120/80 mmHg or lower blood pressure reading is considered normal. However, when the systolic pressure consistently exceeds 130 mmHg and/or the diastolic pressure consistently exceeds 80 mmHg, it indicates the presence of high blood pressure. Hypertension strains the heart and blood vessels, increasing the risk of serious cardiovascular complications, including heart attacks, strokes, and heart failure.
It’s important to note that we don’t solely rely on isolated readings when evaluating blood pressure. Instead, we look for trends over several weeks to understand whether blood pressure remains consistently elevated. This helps us determine if blood pressure is raised sustainably rather than just temporary spikes. By analyzing the long-term trend, we can make more accurate assessments and decisions regarding managing hypertension and its associated risks. Regular blood pressure monitoring and tracking over time provide valuable insights for effective treatment and prevention strategies. Find our Heart Matters BP chart, where you can record your readings and share them with your healthcare professional BLOOD PRESSURE CHART.
High Cholesterol
When discussing high cholesterol, it is important to recognize that cholesterol is a normal and vital component within our bodies. Cholesterol is crucial in various bodily functions, including hormone production, cell membrane formation, and bile acid synthesis. It is transported through the bloodstream in lipoproteins, including low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
However, problems arise when there is an imbalance in cholesterol levels, particularly when LDL cholesterol levels become elevated. LDL cholesterol is often called “bad” cholesterol because it can contribute to plaque buildup in the arteries, leading to atherosclerosis and increasing the risk of heart disease.
Maintaining a healthy balance of cholesterol is essential for optimal heart health. While our bodies naturally produce cholesterol, dietary intake also influences it. Consuming excessive amounts of saturated and trans fats in our diet can raise LDL cholesterol levels and negatively impact cardiovascular health.
Understanding the significance of cholesterol as a vital component allows us to focus on managing and maintaining healthy levels through lifestyle modifications, including a heart-healthy diet, regular exercise, and, if necessary, medication prescribed by healthcare professionals. By striking the right balance, we can ensure that cholesterol continues to serve its essential functions while reducing the risk of heart disease.
Smoking
When addressing smoking and the path to quitting, I understand why many in our community smoke. Smoking can become a habit and an addiction, seemingly offering relief during stress or when calming nerves. It’s a short-term coping mechanism. As a cardiologist, I approach this empathetically. I recognize smoking’s deep roots in personal experiences, social interactions, and emotions.
Cigarette smoke contains harmful chemicals damaging blood vessel linings, causing inflammation and speeding up artery plaque formation, significantly increasing heart disease, heart attacks, strokes, and other health risks. Despite the challenges, I encourage gradual reductions in tobacco use or quitting. It’s a significant step toward better heart health and overall well-being.
Smokers should seek support from healthcare professionals, support groups, or cessation programs. They provide tools, strategies, and resources for this challenging but rewarding journey. Quitting benefits your heart and reduces secondhand smoke exposure to those around you.
After quitting, heart rate and blood pressure drop within hours, reducing cardiovascular strain. Continuing, your body heals. In days to weeks, lung function improves, leading to better oxygen exchange, increased lung capacity, enhanced endurance, improved physical performance, and reduced breathlessness during activities.
The benefits continue. A year after quitting, heart disease risk significantly decreases. Blood vessel lining inflammation diminishes, making it harder for plaque to accumulate, reducing atherosclerosis, heart attacks, and strokes.
Over time, as your smoke-free journey advances, your cardiovascular disease risk keeps decreasing. Long-term studies show that after 5 to 10 years, your heart disease risk approaches that of a nonsmoker.
Diabetes
Diabetes is a chronic medical condition characterized by high blood glucose (sugar) levels. It occurs when the body either does not produce enough insulin (a hormone that regulates blood sugar) or cannot effectively use the insulin it produces. Insulin is vital for transporting glucose from the bloodstream into cells, which is utilized as an energy source. Without proper insulin function, glucose accumulates in the blood, leading to hyperglycemia (high blood sugar levels).
There are different types of diabetes, the most common being type 1 diabetes (often diagnosed in childhood or adolescence) and type 2 diabetes (usually diagnosed in adulthood, often associated with lifestyle factors). Diabetes requires ongoing management, including monitoring blood sugar levels, adopting a healthy diet, engaging in regular physical activity, and, in some cases, taking medication or insulin to maintain stable blood sugar levels. Effective diabetes management is crucial for preventing complications and promoting overall well-being.
Diabetes, specifically type 2 diabetes, often coexists with other risk factors such as obesity, high blood pressure, and high cholesterol levels, collectively known as metabolic syndrome. This combination of factors further elevates the risk of cardiovascular diseases.

The link between diabetes and cardiovascular health lies in the impact of high blood sugar levels on blood vessels. Over time, elevated blood sugar can cause damage to the delicate lining of arteries, promoting the formation of fatty plaques and narrowing the blood vessels. This process, known as atherosclerosis, can impede blood flow and lead to serious cardiovascular events.
Obesity
Obesity is a significant cardiac risk factor, demanding careful attention due to its complex impact on cardiovascular health. Besides affecting physical appearance, it is linked to various metabolic conditions, including diabetes and heightening heart disease risk.
The connection between obesity and cardiovascular health involves multiple factors. Excessive body weight, especially abdominal visceral fat, leads to insulin resistance, reducing cells’ response to insulin, raising blood sugar levels, and causing type 2 diabetes. Diabetes significantly elevates the risk of heart-related issues.
Additionally, obesity strains the heart by increasing its workload. The excess weight forces the heart to pump harder, potentially causing high blood pressure, heart failure, and irregular heart rhythms over time.
Obesity often coexists with other health problems, like obstructive sleep apnea (OSA). OSA, characterized by interrupted breathing during sleep, leads to poor oxygen levels and fragmented sleep. The link between obesity and OSA is significant, as excess weight narrows airways and worsens sleep-related breathing difficulties. OSA, in turn, heightens the risk of cardiovascular problems, including hypertension and heart disease.
Empathy and understanding are crucial when addressing obesity. It’s a complex condition influenced by genetics, hormones, mental health, socioeconomic status, and lifestyle choices. Recognizing its multifaceted nature allows for comprehensive support and personalized interventions to address root causes and promote long-term weight management.
A holistic approach to tackling obesity is essential, encompassing lifestyle changes like adopting a balanced diet, increasing physical activity, and seeking professional guidance. Addressing mental health concerns, fostering a supportive environment, and promoting self-care are vital aspects of effective obesity management.
Excessive alcohol consumption
The impact of alcohol consumption on heart disease is a topic that requires careful consideration. While certain studies have highlighted the potential benefits of moderate alcohol intake, particularly red wine, due to its antioxidant properties and potential impact on blood clotting, it is essential to understand the fine balance between potential benefits and the risks associated with alcohol consumption.
Moderate alcohol intake, one drink per day for women and up to two drinks per day for men has been associated with a lower risk of coronary artery disease. The antioxidants in red wine, such as resveratrol, have shown some potential to promote heart health. However, it is crucial to emphasize the importance of moderation.
Excessive alcohol consumption, on the other hand, can have a detrimental impact on cardiovascular health. Binge drinking or chronic heavy drinking significantly increases the risk of heart disease. It can lead to high blood pressure, weaken heart muscles, and contribute to the development of arrhythmias (abnormal heart rhythms). Additionally, excessive alcohol intake often goes hand-in-hand with an unhealthy lifestyle, including poor dietary choices, smoking, and other risk-taking behaviors, further compounding the cardiovascular risks.
The key message here is moderation and balance. While some studies suggest potential benefits of moderate alcohol consumption, it is essential to be mindful of the associated risks and make informed choices that promote overall cardiovascular well-being. Prioritizing a healthy lifestyle, including maintaining a nutritious diet, engaging in regular exercise, and avoiding tobacco and excessive alcohol consumption, remains the cornerstone of heart disease prevention.
Sedentary Lifestyle
Regarding a sedentary lifestyle and its impact on heart health, it’s important to recognize that small, incremental steps can make a significant difference. While some societies may specify a set amount of exercise per day or week, I believe in working with my patients to set realistic goals tailored to their needs and capabilities.
Embarking on a sudden, intense exercise regimen can be overwhelming and unsustainable for many individuals. Instead, I encourage my patients to start with manageable activities that they enjoy and gradually increase their level of physical activity over time. This approach ensures they are likelier to stick with their exercise routine and reduces the risk of injury or burnout.
It’s essential to acknowledge that some individuals may have underlying medical conditions or physical limitations that restrict their ability to engage in certain types of exercise. In such cases, low-impact activities can be incredibly beneficial. Walking, swimming, cycling, or even chair exercises can provide cardiovascular benefits while minimizing stress on joints or muscles.
In addition to cardiovascular benefits, exercise offers a range of positive effects, including improved mood, increased energy levels, better sleep quality, and enhanced overall well-being. By focusing on small, realistic goals and celebrating each milestone achieved, patients are more likely to maintain a long-term commitment to regular physical activity.
Conclusion
In conclusion, understanding and addressing cardiovascular risk factors are vital to safeguarding our heart health. While some risk factors are beyond our control, such as age and genetics, there are numerous lifestyle factors that we can actively manage. By paying attention to factors such as high blood pressure, cholesterol levels, family history, smoking, obesity, diabetes, alcohol consumption, sedentary lifestyle, and age, we can make informed decisions and take proactive steps to reduce our long-term cardiovascular risks. It is essential to remember that small changes, made consistently over time, can significantly impact our heart health.



