An echocardiogram, often referred to as an “echo,” is a fundamental diagnostic tool in the field of cardiology. This non-invasive procedure harnesses the power of sound waves to provide a comprehensive assessment of the heart’s structure and function. Widely utilized by healthcare professionals, the echocardiogram is an invaluable resource for diagnosing and monitoring a spectrum of cardiac conditions. This article delves into echocardiography, shedding light on its significance in heart health.
How is an Echocardiogram Performed?
The procedure involves using a small transducer, which resembles a handheld device and is placed on the chest. The sonographer performing the test carefully positions the transducer so that it is directed toward the heart. Several different views are acquired from different positions around the chest wall.

Sound Waves Unveiling the Heart’s Secrets
The magic behind an echocardiogram lies in the high-frequency sound waves emitted by the transducer. These sound waves, which are beyond the range of human hearing, serve as the silent messengers of cardiac health. When the transducer releases these sound waves, they travel through the patient’s chest and ultimately reach the heart.
Echoes Paint a Picture
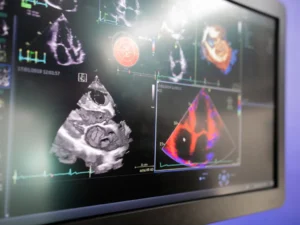
These sound waves bounce back or “echo” to the transducer as they contact the heart’s structures. This is where the true marvel of echocardiography unfolds. The transducer skillfully captures the returning echoes and transforms them into real-time images displayed on a monitor.
Revealing the Heart’s Inner Workings
The images generated during an echocardiogram give clinicians an unparalleled view of the heart’s inner workings. These images vividly showcase the heart’s chambers, valves, and the dynamic flow of blood through the organ. This comprehensive visual data is invaluable in assessing the heart’s overall health, enabling healthcare professionals to detect potential abnormalities or issues.
There are several different applications of echocardiograms, each with its purpose and benefits. Some common types include:
- Transthoracic Echocardiogram (TTE): Among the most commonly performed echocardiograms, TTE is conducted by placing the transducer directly on the skin over the chest. This approach offers a comprehensive view of the heart’s structure and function. TTE is a versatile and widely utilized diagnostic tool, providing valuable insights into cardiac health.
- Stress Echocardiogram: Combining the power of an echocardiogram with either exercise or medication that induces stress on the heart, this test allows healthcare professionals to assess how the heart responds under duress. Stress echocardiograms are invaluable for evaluating the heart’s performance during increased demand, diagnosing conditions such as coronary artery disease, or assessing the effectiveness of treatment plans.
- Transesophageal Echocardiogram (TEE): This specialized echocardiogram involves the insertion of a slender tube equipped with a transducer down the throat and into the esophagus, which is positioned adjacent to the heart. This shares some principles with endoscopy, such as using a flexible tube inserted through the throat. However, it’s important to clarify that while TEE and endoscopy have similarities in their approach, their primary objectives and focus areas are distinctly different. The TEE aims to obtain a highly detailed image of the heart’s internal structures, particularly of the heart valves. TEE is typically employed when a clear and precise image is required or in cases where a standard Transthoracic Echocardiogram (TTE) may not provide the necessary level of detail.
Risks of Echocardiography
Echocardiography, a widely utilized diagnostic modality, relies on harmless ultrasound sound waves to provide detailed cardiac imaging without radiation exposure.
However, the nature of potential risks associated with echocardiography varies based on the specific procedure:
Transthoracic Echocardiogram (TTE): Typically, this procedure is painless and takes around 30 minutes to complete. Occasionally, when the sonographer requires firmer pressure to optimize image quality, individuals may experience momentary discomfort in the area of the chest where the probe is applied.
Transesophageal Echocardiogram (TEE): While transesophageal echocardiograms (TEEs) are generally considered safe and well-tolerated, it’s important to be aware of potential risks associated with this procedure. Patients may experience temporary throat soreness following the test, and in rare cases, the tube used during TEE may cause minor irritation to the throat’s interior. There is also a slight risk of difficulties in swallowing or temporary hoarseness. Additionally, some patients may encounter muscular spasms affecting the throat or lungs and minor bleeding in the throat region. Although uncommon, teeth, gums, or lips injuries have been reported. A rare yet serious complication involves esophageal perforation, characterized by the formation of a hole in the esophagus. Before undergoing a TEE, your doctor will take the time to discuss the potential risks and the benefits of the procedure, ensuring that you are well informed and comfortable with the decision.

Conclusion
In summary, echocardiography is a pivotal diagnostic modality in cardiology, providing essential insights into cardiac structure and function. Through procedures like Transthoracic Echocardiograms (TTE), Transesophageal Echocardiograms (TEE), and Stress Echocardiograms, healthcare professionals gain crucial data for diagnosing and managing cardiac conditions. Echocardiography’s non-invasive, radiation-free nature and real-time imaging capabilities underscore its importance in cardiac health. As cardiology advances, echocardiography plays a central role in improving patient outcomes and our understanding of heart health.


