As a cardiologist, I often help patients understand their conditions by explaining how their heart functions. This helps simplify complex medical concepts, making them more accessible. This approach empowers individuals to grasp the impact of their conditions and the rationale behind various treatments. Similarly, the upcoming article on cardiac anatomy and physiology aims to demystify the intricate workings of the heart, providing readers with a clearer insight into this vital organ’s functions. The article will empower readers to make informed decisions about their cardiovascular health and well-being by breaking down these complexities. Don’t forget to explore our Heart Works page to delve deeper into the marvel of our cardiac system. Access it by clicking here.
Overview of the Human Heart Anatomy and Physiology
The human heart, a complex organ, circulates blood throughout the body. This muscular organ propels oxygenated and deoxygenated blood to and from the lungs and the rest of the body. It consists of four chambers: the right atrium, left atrium, right ventricle, and left ventricle.
Chambers
The right atrium receives deoxygenated blood from the body and transfers it to the right ventricle. Subsequently, the right ventricle propels the deoxygenated blood to the lungs, which undergoes oxygenation. The oxygenated blood then returns to the left atrium, which propels it to the left ventricle. Finally, the left ventricle pumps the oxygenated blood to the body’s tissues and organs.
Pericardium, myocardium and endocardium
The heart comprises three layers: the pericardium, the myocardium, and the endocardium. The pericardium is the outermost layer and comprises a thin layer of connective tissue. The myocardium is the middle layer and is composed of cardiac muscle. The endocardium is the innermost layer and is composed of endothelial cells. Conditions like pericarditis involve inflammation of the pericardial layer, while myocarditis affects the heart muscle.
Heart valves
The heart is also composed of four valves: the tricuspid valve, the pulmonary valve, the mitral valve, and the aortic valve. The tricuspid valve is located between the right atrium and the right ventricle and prevents the backflow of blood from the right ventricle to the right atrium. The pulmonary valve is located between the right ventricle and the pulmonary artery and prevents the backflow of blood from the pulmonary artery to the right ventricle. The mitral valve is located between the left atrium and the left ventricle and prevents the backflow of blood from the left ventricle to the left atrium. The aortic valve is located between the left ventricle and the aorta and prevents the backflow of blood from the aorta to the left ventricle.
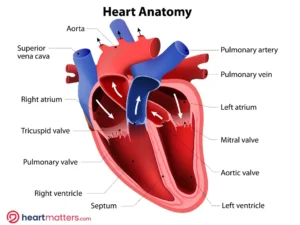
This image presents a depiction of the human heart’s internal structure. It illustrates the chambers, valves, and blood vessels that make up this vital organ. The diagram focuses on the atria, ventricles, and the network of arteries and veins responsible for circulating blood.
The heart is also composed of several electrical conduction pathways that control the rhythm of the heartbeat. The sinoatrial node, or SA node, is the heart’s natural pacemaker and is located in the right atrium. The SA node produces electrical impulses that travel through the atria and cause them to contract. The electrical impulses then travel through the atrioventricular node, or AV node, located in the interatrial septum, and then to the ventricles, causing them to contract.
Cardiac Muscle Structure and Function
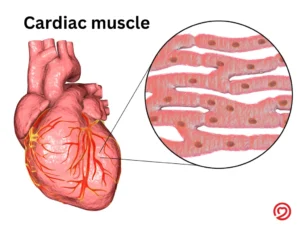
Cardiac muscle, an involuntary tissue within the heart’s walls, propels rhythmic contractions that circulate blood throughout the body. Comprising elongated, branched cells interconnected by intercalated discs, this specialized tissue features gap junctions for swift electrical signal transmission. These signals orchestrate the synchronized heart contractions that generate the heartbeat.
Furthermore, these cardiac muscle cells are highly specialized for their role. They are enveloped by the sarcolemma, which is enriched with signal-receiving proteins. Abundant mitochondria within provide cellular energy, while unique myosin proteins fuel contractions.
In addition, pacemaker cells confer independent contractility upon cardiac muscle cells, generating electrical impulses that unify heart contractions. Hormones like adrenaline and neurotransmitters like acetylcholine modulate heart rate, responding to various stimuli.
Moreover, the autonomic nervous system, which governs involuntary functions, plays a significant role in regulating cardiac muscle contractions. This system finely adjusts heart rate in response to stimuli. Vital for life, cardiac muscle effectively pumps blood, delivering the body with essential oxygen and nutrients.
Blood Flow Through the Heart
The heart, a vital organ, propels blood throughout the body, maintaining proper function. Blood flow is divided into two key processes: pulmonary circulation and systemic circulation.
Pulmonary circulation involves blood movement from the heart to the lungs and back. Blood departs the right heart chamber, travels to the lungs for oxygenation, and returns to the left side for distribution.
Systemic circulation moves blood from the heart to the body and back. Oxygenated blood from the left side flows to the body before returning to the right side for eventual oxygenation.
Pulmonary and aortic valves link the circulations, governing blood flow direction. The heart’s four chambers – right atrium, left atrium, right ventricle, and left ventricle – operate in synergy. The right atrium pumps deoxygenated blood to the right ventricle, which sends it to the lungs. The left atrium transfers oxygenated blood to the left ventricle, which dispatches it to the body.
This intricate blood flow sustains proper bodily function. The heart oxygenates blood for the body and lungs, guided by the pulmonary and aortic valves. The collaborative effort of the four chambers ensures efficient blood oxygenation and distribution.
Cardiac Conduction System and Electrical Activity
The cardiac conduction system is a group of specialized cells in the heart that generate and conduct electrical impulses. These electrical impulses travel through the heart, causing it to contract and pump blood throughout the body. The cardiac conduction system is responsible for initiating and coordinating the electrical activity of the heart, which is essential for the proper functioning of the cardiovascular system.
The cardiac conduction system consists of three main components: the sinoatrial (SA) node, the atrioventricular (AV) node, and the bundle of His. The SA node is located in the upper right chamber of the heart, the right atrium. It is the heart’s natural pacemaker, generating electrical impulses that travel throughout the heart. The AV node is located in the lower right chamber of the heart, the right ventricle. It receives the electrical impulses from the SA node and delays them before sending them to the bundle of His. The bundle of His is a group of specialized cells located in the septum between the right and left ventricles. It receives the electrical impulses from the AV node and conducts them to the ventricles, causing them to contract and pump blood throughout the body.
The electrical activity of the heart is measured by an electrocardiogram (ECG). An ECG records the electrical activity of the heart as it contracts and relaxes. It is used to diagnose heart conditions and monitor the effectiveness of treatments.
The cardiac conduction system is essential for the proper functioning of the cardiovascular system. Without it, the heart would not be able to pump blood throughout the body, resulting in death. Therefore, it is important to maintain a healthy cardiac conduction system in order to ensure the proper functioning of the cardiovascular system.
The Heart Valves
The heart is an organ responsible for pumping blood throughout the body. It is composed of four chambers, two atria and two ventricles, and four valves. The valves are responsible for controlling the flow of blood through the heart. They open and close to ensure that blood flows in the correct direction.
The four valves of the heart—namely, the tricuspid, pulmonary, mitral, and aortic valves—each serve a crucial purpose. The tricuspid valve, positioned between the right atrium and right ventricle, prevents blood from regressing into the right atrium during the right ventricle’s contraction. Similarly, the pulmonary valve, situated between the right ventricle and the pulmonary artery, halts backflow as the pulmonary artery contracts. The mitral valve, located between the left atrium and left ventricle, ensures blood doesn’t return to the left atrium during the left ventricle’s contraction. Lastly, the aortic valve, situated between the left ventricle and the aorta, maintains unidirectional blood flow as the aorta contracts.
This intricate orchestration of heart valves is pivotal for optimal cardiac function. Their synchronized opening and closing mechanism guarantees proper blood flow direction. When the heart contracts, valves open to facilitate outward blood flow. Conversely, during relaxation, valves promptly seal to avert backflow. This seamless interplay ensures efficient circulation of blood throughout the body, maintaining optimal function.
Heart valves actively maintain pressure during heart contractions. As the heart contracts, these valves open, facilitating the exit of blood and contributing to increased pressure for efficient circulation. Conversely, when the heart relaxes, the valves promptly close to prevent backflow. This closure not only prevents blood from flowing back but also reduces pressure, serving as a safeguard against overexertion.
These valves are vital for optimal cardiac performance. Their synchronized operation ensures proper blood flow direction and pressure regulation, enabling efficient circulation. Without them, the heart’s ability to effectively pump blood throughout the body would be compromised.
Conclusion
In conclusion, the heart is a fascinating organ with a complex anatomy and physiology. It is responsible for pumping blood throughout the body, delivering oxygen and nutrients to every cell, and removing waste products. The heart consists of four chambers, valves, and a network of blood vessels that work together to ensure efficient circulation. Understanding the cardiac anatomy and physiology is crucial for diagnosing and treating cardiovascular diseases, which remain a leading cause of mortality worldwide. By appreciating the remarkable complexity and elegance of the heart’s structure and function, we can gain a deeper appreciation for the marvels of the human body. For further information, visit our Heart Works page!


