Supraventricular tachycardia (SVT) is a condition marked by rapid heart rates originating in the upper heart chambers known as the atria. Spanning across all age groups, SVT triggers palpitations, breathlessness, and a fluttering sensation in the chest. A recent study, published in the Lancet medical journal, called the RAPID trial, heralds encouraging strides in the realm of SVT management, showcasing the potential of a self-administered intranasal medication called etripamil for rapidly converting SVT to a normal heart rhythm in the community, outside the healthcare setting at the time of onset of this condition [1].
Understanding SVT
Supraventricular Tachycardia (SVT) entails rapid bursts of heartbeats stemming from the atria, leading to abnormally accelerated rates – often exceeding the typical resting heart rate. This sparks palpitations, chest flutters, shortness of breath, and occasional mild dizziness. SVT’s origin lies in irregular electrical pathways or circuits within the heart, spurring swift impulses that unsettle the heart’s rhythm. While SVT is generally non-life-threatening, it’s disconcerting and inconvenient for those grappling with it. SVT episodes can be brief or protracted, varying from seconds to minutes or more.
SVT’s triggers and root causes are multifaceted. Activities, emotions, and stimuli like caffeine or stress may set it off. Others might experience SVT due to underlying heart issues or structural anomalies in the heart’s electrical system. Seeking medical evaluation when SVT symptoms arise is crucial. Healthcare providers diagnose SVT via tests like electrocardiograms (ECGs) and Holter monitors. SVT management encompasses an array of approaches, including lifestyle adjustments, medications, or invasive procedures like catheter ablation or cardioversion – contingent on episode frequency and severity.

Managing Acute SVT Attacks
When SVT thrusts heart rates at very fast rates, frequently more than 150 bpm during acute attacks, the conventional response entails seeking prompt medical care if the heart doesn’t naturally revert to a normal rhythm post-techniques like the Valsalva maneuver (bearing down while holding your breath, stimulating the vagus nerve to restore rhythm). In ambulances or emergency departments, adenosine – a swift-acting intravenous medication – assumes center stage, aiding heart rate normalization. If unsuccessful, controlled electric shocks or cardioversion might be considered to reset the rhythm.

In some cases when the heart rate is not slowing down, it may be necessary to perform an emergency procedure known as a cardioversion. It involves delivering a controlled electric shock to the heart, typically under anesthesia, to reset its rhythm and allow it to resume beating in a coordinated and regular pattern.
New Study Unveils Promise
The RAPID Study: RAPID, a multicenter trial across 160 North American and European sites, assessed etripamil nasal spray’s safety and efficacy for paroxysmal supraventricular tachycardia (PSVT) treatment [1b]. Etripamil outperformed the placebo in swiftly converting PSVT cases to a normal heart rhythm. Etripamil users noted better heart rhythm improvement compared to placebo users. Etripamil’s effectiveness surfaced within 30 minutes and sustained for up to 300 minutes – even outside healthcare settings within the community. Etripamil is a fast-acting, intranasally administered calcium-channel blocker in development for on-demand therapy outside a health-care setting for paroxysmal supraventricular tachycardia. The investigators aimed to evaluate the efficacy and safety of etripamil 70 mg nasal spray using a symptom-prompted, repeat-dose regimen for acute conversion of SVT to normal regular sinus rhythm within 30 min.
Optional Repeat-Dose Approach: The study also explored an optional-repeat-dose approach, where patients could administer a second dose of etripamil if their symptoms persisted. This approach further enhanced the efficacy of etripamil in converting PSVT to a normal heart rhythm [2]. This finding suggests that patients have the potential to manage their own PSVT episodes with self-administered etripamil, reducing the need for additional medical interventions.
Self-Administered Etripamil’s Advantages: Self-administered etripamil grants patients command over their PSVT episodes. With the nasal spray at hand, symptom management becomes swift and convenient at episode onset.
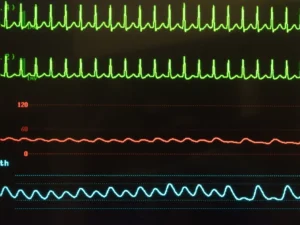
SVT is characterized by a very fast (often > 150bpm) heart rate that is regular. The electrocardiogram has a characteristic pattern that can be quickly identified and allows prompt treatment to be provided
Deeper Dive into Etripamil
Etripamil, a calcium channel blocker, caters to rapid treatment for specific heart rhythm disorders, chiefly PSVT. Administered intranasally, the nose spray ensures swift absorption and rapid action. Blocking heart calcium channels regulates electrical signals that control heartbeat, aiding the return to normal rhythm during PSVT. Etripamil’s on-demand use targets PSVT episodes, averting invasive interventions during acute care.
The RAPID study illuminates etripamil’s efficacy and safety for PSVT treatment. It underscores etripamil’s potential in converting PSVT to normal rhythm, empowering patients to manage their episodes. As research advances, etripamil holds promise as a valuable clinical treatment, lightening the PSVT healthcare burden. Etripamil is emblematic of medical progress, offering innovative solutions that grant patients control and convenience in addressing medical needs. Stay tuned for more updates in this evolving landscape.
[1] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)00776-6/fulltext


