If you’ve recently experienced a heart attack, navigating the road to recovery may seem daunting. However, this challenging period can significantly improve your overall well-being with the right approach.
This article explores the steps you can take to facilitate your recovery journey. From prioritizing proper medical care to implementing lifestyle adjustments and seeking support from your loved ones, each action is crucial in enhancing your heart health. By understanding the importance of these measures and committing to them wholeheartedly, you can approach your recovery with confidence and optimism, knowing that each step brings you closer to a better quality of life.
What is a heart attack?
A heart attack, also known as a myocardial infarction (MI), is a critical medical event when blood flow to a section of the heart muscle is significantly reduced or blocked. This reduction in blood flow deprives the heart muscle of oxygen and nutrients, damaging the heart tissue. Prompt medical attention is crucial during a heart attack to minimize the extent of damage and improve the chances of recovery.
Classification of Heart Attacks: NSTEMI and STEMI
When discussing heart attacks, it’s common to differentiate between two main types: ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI). While STEMI is often perceived as the more severe form due to its immediate and obvious ECG changes, it’s crucial to recognize that both STEMI and NSTEMI are significant and can have serious implications.
STEMI is marked by a complete coronary artery blockage, which suddenly disrupts blood flow to a portion of the heart muscle. This results in immediate and characteristic changes on an electrocardiogram (ECG), demanding swift intervention to restore blood flow and minimize heart damage.
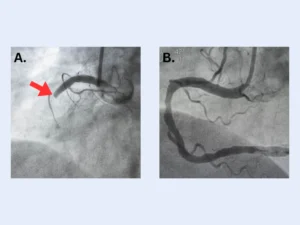
An example of a STEMI heart attack is seen during a coronary angiogram. A: Pre-Intervention angiogram – The left panel illustrates a critical scenario involving an acute heart attack within the right coronary artery. The red arrow designates a complete blockage, which impedes blood flow downstream from the obstruction. This blockage primarily comprises a clot and necessitates immediate emergency intervention to reinstate unobstructed blood circulation. B: Post-Intervention angiogram – The right panel depicts the same coronary artery after a successful treatment. A stent has been deployed to address the blockage, and the image showcases the restored size and patency of the artery. This post-treatment result highlights the efficacious blockage management, leading to the resumption of normal blood flow within the artery.
NSTEMI, on the other hand, involves a partial blockage of a coronary artery, which can trigger less pronounced ECG changes. Despite the absence of certain ECG patterns associated with STEMI, NSTEMI remains a major heart event that necessitates rapid assessment and medical attention to prevent further damage.
While STEMI often captures more attention due to its distinct ECG changes, both types of heart attacks require urgent medical intervention. The key lies in promptly identifying the type of heart attack and tailoring appropriate treatments to minimize heart muscle damage and improve long-term outcomes.
Regardless of the type of heart attack you’ve experienced, it’s highly probable that you’ve undergone stent placement to address the blockage, in addition to commencing a regimen of various medications.
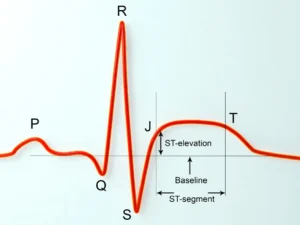
This figure illustrates an electrocardiogram (ECG) highlighting the ST segment. The ST segment is a critical component of the ECG waveform to differentiate between ST-elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI) cases.
Acknowledging Your Emotions
Leaving the hospital environment and transitioning back home can trigger various emotions. Understand that feeling anxious, uncertain, or even overwhelmed during this time is expected. Recognize and accept your feelings, allowing yourself the space to process them. Remember, healing involves not only physical aspects but also emotional well-being.
Building a Support Network
Your loved ones may also experience concerns and uncertainties about how to support you on your road to recovery. Foster open communication with your family and friends, sharing your feelings and needs. During this phase, you can establish a support network that encourages and uplifts you. Their presence and understanding will provide a tremendous source of strength.
Self-Care and Lifestyle Adjustments
Recovering from a heart attack necessitates making positive lifestyle changes. Embrace this as an opportunity to prioritize self-care and adopt heart-healthy habits. Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Engage in regular physical activity as recommended by your healthcare provider. Adequate sleep, stress management techniques, and avoiding tobacco and excessive alcohol consumption are also crucial for your recovery.
Medication compliance

Recovering after a heart attack is a critical journey that demands physical and emotional strength. One aspect that requires our utmost attention is the post-discharge medication regimen. For many, this could be their first encounter with a regular medication routine, and the prospect can feel overwhelming. It’s normal to have mixed emotions and questions, especially when faced with multiple prescriptions to aid recovery. Remember, you’re not alone in this. Your healthcare team and pharmacist are invaluable resources ready to guide you through the process.
It is crucial to engage in open conversations about your medications, their purposes, potential side effects, and any concerns you may have. These medications have been carefully chosen to support your heart’s healing journey, and taking them as directed will significantly enhance your recovery prospects. As you navigate this new chapter, the key lies in remaining compliant with your medication schedule. Feeling uncertain at first is alright, but you’ll become more confident in managing your regimen with time. Your well-being is a priority, a significant step towards regaining your health and leading a fulfilling life.
Gradual Physical Activity
Consult your healthcare provider about a suitable exercise plan tailored to your needs. Engage in cardiac rehabilitation programs that guide you through safe and gradual physical activities. Exercise strengthens your heart, boosts your mood, reduces stress, and enhances overall well-being. Start with light activities and gradually progress under professional guidance.
Progressing after a heart attack signifies triumph, underscoring the potential for healing and exemplifying your resilience. Embrace this path as a fresh start, a chance to collaboratively shape positive lifestyle adjustments with your healthcare team, leading to improved well-being and vitality.
Embracing a Positive Mindset
Maintaining a positive mindset is instrumental in your recovery. Focus on the progress you have made, no matter how small. Celebrate your accomplishments and milestones along the way. Surround yourself with positive influences, whether uplifting music, inspiring books, or engaging in hobbies that bring you joy. Cultivate gratitude for each day and appreciate the second chance at life.

Cardiac rehabilitation programs after discharge encompass supervised exercises, dietary guidance, and lifestyle modifications. This comprehensive approach aims to enhance cardiovascular health, promote recovery, and improve overall well-being.
Seek Professional Support
If you struggle with anxiety, depression, or any emotional challenges, do not hesitate to seek professional help. Mental health professionals can provide valuable guidance and support tailored to your needs. They will help you navigate your emotions and equip you with coping strategies to thrive during your recovery.
Conclusion
The recovery journey following a heart attack can indeed be daunting and uncertain, not only for you but also for your loved ones. From grappling with limitations on what you can do to managing medication side effects, it’s natural to feel anxious. However, there are numerous resources available to support you during this phase. Your local healthcare professional, hospital cardiology units, rehabilitation programs, and pharmacists can all provide valuable assistance.
It’s important to take each day as it comes without rushing the process. Listen to your body and do what feels manageable. Cultivating a positive mindset can help ease anxieties, and as you progress, the future holds promise for brighter days ahead.
Other useful resources:
American College of Cardiology (ACC):
American Heart Association (AHA):
European Society of Cardiology (ESC):
Heart Attack (Myocardial Infarction) Information
British Heart Foundation:



