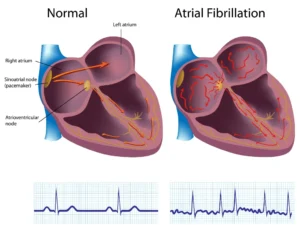
Atrial fibrillation (AF) is familiar in clinical practice and impacts millions worldwide. Interestingly, many individuals may remain asymptomatic, incidentally diagnosed during routine checks like pulse assessments, electrocardiograms (ECGs), or heart monitor analyses. If you’re interested in a comprehensive exploration of AF and its connection to stroke risk assessment, our informative article is just a click away here.
If you have been diagnosed with AF, let’s look at some of the treatment options available that your healthcare professional will discuss with you. Let’s start by discussing the non-medical options, which are fundamental for all individuals dealing with AF. These strategies focus on lifestyle modifications and proactive management of underlying factors.

Lifestyle Adjustments
Lifestyle changes play a pivotal role in managing AF effectively. These changes encompass:
- Smoking Cessation: If you’re a smoker, quitting is imperative. Smoking is linked to a higher risk of heart disease and exacerbates AF symptoms.
- Alcohol Moderation: Reducing alcohol consumption is advisable, as excessive intake can trigger AF episodes. Practicing moderation can positively impact your heart’s rhythm. An unmistakable link exists between regular and excessive alcohol consumption and the onset of AF. It’s a scenario we often encounter: individuals enjoying a night out on a Saturday, indulging in a few drinks, only to find themselves in the Emergency Department (ED) later, experiencing rapid AF for the first time. This occurrence underscores the immediate impact that alcohol can have on heart rhythm, and it serves as a poignant reminder of the need for moderation in alcohol intake for those living with or at risk of AF.
- Healthy Diet: Embrace a heart-healthy diet rich in vegetables, whole grains, lean proteins, and healthy fats. This dietary approach supports overall cardiovascular health. For more information on this, please check out our article here.
- Physical Activity: Regular exercise can help maintain a healthy weight and improve cardiovascular fitness. Discuss an appropriate exercise plan with your healthcare provider. See our article here for more information.
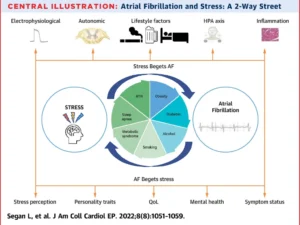
- Stress Management: Acute and chronic stress can contribute to AF episodes. This is nicely explained in a recent publication by Segan L et al, in J Am Coll Cardiol EP. 2022 Aug, 8 (8) 1051–1059.
As depicted in the figure, atrial fibrillation (AF) and stress share a complex and bidirectional relationship. Stress exerts significant direct physiological effects on the heart, represented by the arrows labeled “Direct Physiological Effects.” This stress-induced impact is further influenced by traditional cardiovascular risk factors like hypertension (HTN), which are indirectly affected by stress, as indicated by the arrows labeled “Indirect Effects through Cardiovascular Risk Factors.” This intricate interplay contributes to the pathogenesis of AF. Conversely, AF can intensify stress perception, potentially leading to depression and diminished overall well-being. This reciprocal relationship underscores the importance of addressing stress in AF management. Source: Segan et al. J Am Coll Cardiol EP. 2022 Aug, 8 (8)
Managing Underlying Factors
Effectively managing underlying health conditions is crucial in AF management:
- Obstructive Sleep Apnea (OSA): If you’ve been diagnosed with obstructive sleep apnea (OSA), addressing it can yield significant improvements in managing AF symptoms. OSA is characterized by interrupted breathing during sleep, which can stress the cardiovascular system and trigger AF episodes. Continuous Positive Airway Pressure (CPAP) therapy is a primary intervention for OSA. CPAP involves wearing a mask during sleep that delivers a continuous flow of air, keeping the airway open. By ensuring uninterrupted breathing patterns, CPAP can alleviate the strain on your heart and reduce the likelihood of AF occurrences.
- Hypertension and Diabetes: Effective management of hypertension (high blood pressure) and diabetes is paramount in AF care. These conditions are interconnected and can exacerbate AF. Elevated blood pressure strains the heart and increases the risk of irregular heart rhythms. Similarly, uncontrolled blood sugar levels in diabetes can contribute to heart complications, including AF. Medications prescribed by your healthcare provider, alongside lifestyle adjustments like a balanced diet, regular exercise, and stress reduction, are pivotal in controlling blood pressure and blood sugar levels. Keeping these factors within healthy ranges enables you to promote stable heart function and minimize the triggers for AF episodes.
- Weight Management: Maintaining a healthy weight offers substantial benefits in AF management. Excess weight increases stress on the heart, making it more prone to irregular rhythms. Even a modest weight reduction can improve heart function and rhythm stability. A well-balanced diet and regular physical activity are key components of effective weight management. Working with your healthcare provider or a registered dietitian to create a personalized plan can help you achieve and sustain a healthy weight. By relieving the heart of unnecessary strain, you’re enhancing its ability to maintain a regular rhythm and minimizing the risk of AF occurrences.
Remember, these aspects are interconnected, and their effective management complements the overall strategy for managing AF. Collaboration with your healthcare provider to tailor interventions to your unique needs and medical history is crucial for optimizing your AF management journey.

Medical Treatment Options for Atrial Fibrillation
Maintaining an appropriate heart rate is essential in AF for alleviating symptoms and preventing complications. This is especially important because in specific individuals, if the heart rate remains excessively high over a prolonged period, it can potentially compromise the heart’s strength and lead to weakening (left ventricular dysfunction). Moreover, it can contribute to worsening symptoms related to congestive heart failure.
Medications to Slow the Heart Rate
Medications known as rate control agents slow the heart rate and improve the heart’s efficiency. Here are some common medications in this category:
Beta-Blockers: These drugs, such as metoprolol, carvedilol, and atenolol, block the effects of adrenaline on the heart. By doing so, they lower the heart rate, reduce the force of heart contractions, and help control symptoms of AF. They help stabilize heart rhythm and are especially effective in patients with rapid heart rates during AF episodes.
Calcium Channel Blockers: These drugs also control heart rate by affecting the flow of calcium into heart cells. They are particularly beneficial for individuals who experience rapid heart rates during AF. Medicines like diltiazem and verapamil work by relaxing blood vessels and reducing the heart’s pumping strength. This leads to a slower heart rate and improved blood flow.
Digoxin: Digoxin enhances the heart’s contractions and slows down electrical signals, resulting in a decreased heart rate. It’s often used in combination with other medications for rate control. You can find more on our dedicated Digoxin article here.
Amiodarone: While primarily used to control heart rhythm, amiodarone also has rate-control properties. It can help reduce the heart rate in cases where other medications are less effective.
Ivabradine: This newer medication inhibits the “funny” current in the heart’s pacemaker cells, slowing the heart rate. Studies on ivabradine’s impact on AF have yielded conflicting results. Some studies suggest that ivabradine could contribute to AF, while others indicate that it led to a moderate rate reduction in patients with permanent AF. The primary mechanism responsible for this reduction seems to inhibit the “funny” current in the atrioventricular node. As a result, further research is required to determine whether recommending ivabradine is advisable.
These medications aim to improve the heart’s efficiency, alleviate symptoms like palpitations and shortness of breath, and enhance cardiovascular function. The choice of medication depends on individual patient factors, including existing medical conditions, potential side effects, and interactions with other drugs. Your healthcare provider will determine the most appropriate rate control agent for your specific needs and closely monitor your response to the treatment.
Medicines to Control the Heart Rhythm
Medications can sustain a regular heart rhythm or strive to restore the heart to its natural sinus rhythm in instances of AF. These pharmaceutical options hold significance in aiding individuals towards this goal; however, their usage requires careful consideration in consultation with a healthcare professional, as specific side effects necessitate vigilant monitoring. It should be noted that not all medications are available in all countries. Some that are used around the world include:
Flecainide: This sodium channel blocker helps stabilize heart rhythms by regulating the flow of sodium ions into heart cells. It is often used to treat AF and certain other arrhythmias.
Propafenone: Like flecainide, propafenone is another sodium channel blocker that helps restore normal heart rhythms and control AF episodes.
Sotalol: This medication combines beta-blocker properties with antiarrhythmic effects, effectively managing AF by controlling heart rate and rhythm.
Amiodarone: Although typically reserved for more severe cases of AF, amiodarone is highly effective in maintaining normal heart rhythm. It works by affecting multiple ion channels in the heart. Although amiodarone is one of the more effective medicines for maintaining a regular rhythm, it is associated with several long-term side effects, especially on the liver, lungs, skin, and thyroid gland.
Dofetilide: This potassium channel blocker helps regulate the flow of potassium ions, maintaining a steady heart rhythm and preventing AF episodes.
It’s important to note that while these medications can effectively control heart rhythm, their usage requires careful monitoring due to potential side effects and interactions with other medicines. Treatment plans should be tailored to individual patient needs, and consultation with a healthcare provider is essential to determine the most suitable antiarrhythmic drug and dosage for managing AF effectively.
Medicines to Prevent Blood Clot Formation
I frequently address patient inquiries regarding the effectiveness of aspirin alone in reducing stroke risk associated with AF. For those diagnosed with AF and identified as having a higher risk of stroke, the recommendation leans towards prescribing anticoagulants like warfarin, dabigatran, apixaban, or rivaroxaban instead of aspirin. This shift away from aspirin arises from a growing body of evidence that highlights the superior efficacy of warfarin and modern anticoagulants in preventing strokes compared to aspirin.
However, it’s essential to recognize that not all AF patients require anticoagulant therapy. Each individual’s risk factors for both stroke and bleeding should be thoroughly assessed, guiding the most suitable course of action. Anticoagulants are prescribed to mitigate the risk of blood clot formation and subsequent stroke. These include:
Warfarin: Warfarin is a traditional anticoagulant that helps prevent blood clots by inhibiting certain clotting factors. Regular monitoring is required.
Direct Oral Anticoagulants (DOACs): These newer anticoagulants, including rivaroxaban, apixaban, dabigatran, and edoxaban, offer effective stroke prevention without frequent monitoring.
It’s important to note that treatment choices should be personalized based on individual health status, risk factors, and preferences. Consultation with a healthcare provider is crucial to determine the most suitable treatment plan for managing AF effectively and reducing the associated risks. Further details can be found in our dedicated article on AF and the risk of stroke by clicking here.

Direct Cardioversion for Atrial Fibrillation
Direct cardioversion remains a valuable medical procedure for swiftly restoring a regular heart rhythm in atrial fibrillation (AF) patients. This method employs controlled electric shocks delivered to the heart through specialized paddles or patches on the chest, strategically timed to synchronize with the heartbeat. However, a crucial precaution is often taken before direct cardioversion to ensure safety and efficacy. Sometimes, a transesophageal echocardiogram (TEE) is performed before cardioversion. This ultrasound test evaluates the heart’s chambers and can identify the presence of any blood clots, which could pose a risk during the procedure. Direct cardioversion might be deferred if a clot is detected until appropriate measures are taken to dissolve or address the clot. This precaution underscores the importance of mitigating potential risks associated with direct cardioversion. By combining TEE testing with direct cardioversion, healthcare providers can maximize the procedure’s benefits while prioritizing patient safety and optimal outcomes. Your healthcare team will determine the necessity of TEE based on your health profile and AF condition. Have a look at our YouTube short on cardioversion for more details here.
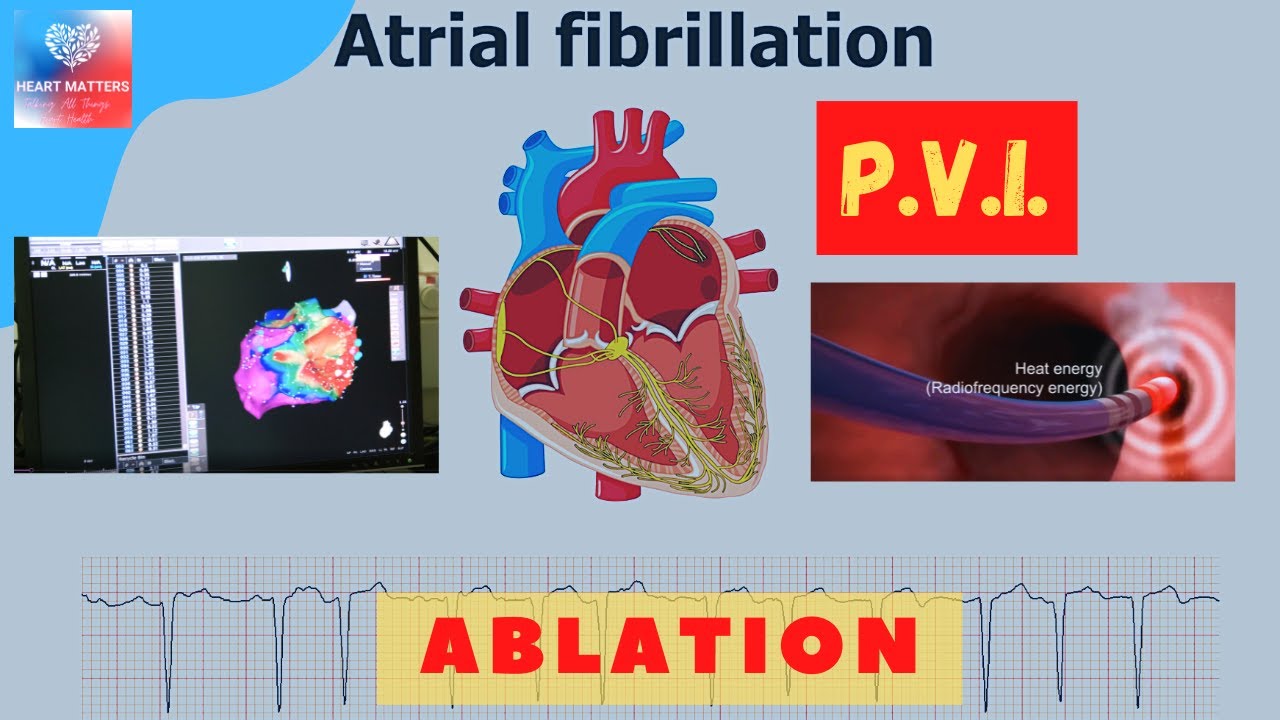
Catheter Ablation Procedure (Pulmonary Vein Isolation)
Catheter ablation, specifically the Pulmonary Vein Isolation (PVI) technique, is a sophisticated procedure for managing AF. During PVI, thin, flexible catheters are threaded through blood vessels and carefully guided to the heart under anesthesia. The targeted objective is to isolate the pulmonary veins, the sites from which abnormal electrical signals often trigger AF.
By creating small scars around the veins through controlled energy delivery, the erratic electrical pathways causing AF can be disrupted. This process, akin to creating “roadblocks” for the irregular signals, aims to restore a steady heart rhythm. PVI is typically performed under localized anesthesia and guided by advanced imaging technology, ensuring precision and minimizing invasiveness.
This procedure is considered when other treatment methods, like medications, have proven less effective. Catheter ablation, particularly PVI, offers individuals with AF the prospect of improved symptom management and an enhanced quality of life. Your healthcare provider will assess your suitability for this procedure based on your unique condition and medical history.
In specific scenarios, patients requiring open heart surgery for arterial blockages or heart valve corrections may benefit from a combined ablation procedure. This approach entails the surgeon performing an ablation during the surgical intervention. While addressing arterial blockages or heart valve issues, the surgeon can simultaneously target and eliminate abnormal heart tissue contributing to AF. This dual-purpose procedure aims to improve the heart’s overall function while addressing the irregular heart rhythm.
Role of Pacemaker Devices in Atrial Fibrillation
In cases where traditional management methods struggle to control fast heart rates effectively, a pacemaker may be considered, often as a last resort. It’s essential to clarify a common misconception: pacemakers don’t directly stop AF. Instead, they serve as a crucial first step in a two-phase approach.
A pacemaker can help maintain a steady and more controlled heart rate when AF leads to extremely rapid and irregular heartbeats. By providing consistent pacing signals, pacemakers ensure that the heart doesn’t race uncontrollably. However, pacemakers alone don’t address the underlying irregular electrical signals causing AF.
A common misconception is that a pacemaker alone can stop AF or control rapid heart rates. However, pacemakers stabilize slow rhythms and are part of a broader strategy alongside other interventions for specific cases. function as part of a comprehensive strategy, working in tandem with other interventions to provide effective management in a select group of people.
In the second phase, AV node ablation may be performed. During AV node ablation, the electrical connection between the upper and lower chambers of the heart is intentionally disrupted. This prevents the chaotic electrical signals from the atria (upper chambers) from reaching the ventricles (lower chambers), effectively controlling the heart rate. After AV node ablation, a permanent pacemaker is required to ensure a stable heart rate since the heart’s natural pacing mechanism is intentionally disrupted.
In this way, pacemakers play a pivotal role in AF management by mitigating the impact of rapid heart rates. However, it’s important to note that they are only part of a comprehensive strategy when other treatments have proven inadequate. Decisions regarding pacemaker implantation and subsequent interventions are made based on each patient’s condition and medical history.
Conclusion
Atrial fibrillation management is highly personalized, with healthcare providers crafting tailored strategies. Whether involving lifestyle changes, medical interventions, or advanced procedures like catheter ablation, each step contributes to better AF control. It’s essential to acknowledge AF’s common occurrence in communities, often presenting without symptoms. In such cases, diligent monitoring and clot risk reduction suffice. Prioritizing communication with healthcare professionals and commitment to effective strategies empower individuals in their AF management journey.