The HbA1c blood test is valuable in assessing and managing diabetes and overall health. In this article, we will delve into what the HbA1c test is, what it tells us about our health, and why it is a valuable marker for individuals with diabetes and those at risk of developing the condition.
What is HbA1c?
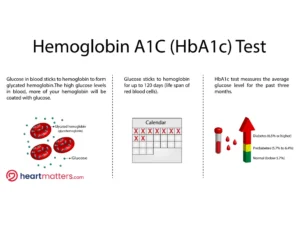
HbA1c, or Hemoglobin A1c, is a blood test that measures the average glucose level in your blood over the past two to three months. It does this by assessing the percentage of hemoglobin (a protein in red blood cells) that is glycated or has glucose attached. The higher the percentage, the higher your average blood sugar levels.
Diabetes Diagnosis and Monitoring
The HbA1c test primarily serves to diagnose and monitor diabetes. Consistently elevated HbA1c levels may indicate diabetes or prediabetes, with a diagnosis typically occurring when the HbA1c level reaches 6.5% or higher. Monitoring HbA1c levels in individuals with diabetes is important, as higher HbA1c levels elevate the risk of developing diabetes-related complications, such as diabetic retinopathy, diabetic kidney disease, and diabetic neuropathy.
Long-term Blood Sugar Control:
The HbA1c test is a useful complementary test to daily glucose monitoring because it provides a broader picture of blood sugar control over several months. This long-term view helps healthcare providers and individuals with diabetes make more informed decisions about treatment and lifestyle adjustments.
Complications Risk Assessment:
Maintaining a healthy HbA1c level is essential in reducing the risk of diabetes-related complications. Elevated HbA1c levels are associated with a higher risk of heart disease, kidney problems, nerve damage, and eye issues. By keeping HbA1c in check, individuals can lower their risk of these complications.
Setting Targets:
For individuals with diabetes, healthcare professionals often set personalized HbA1c targets to achieve optimal blood sugar control. These targets vary depending on age, overall health, and other medical conditions. Achieving and maintaining these targets is vital for preventing complications.
Conclusion
The HbA1c blood test provides valuable insights into our blood sugar control and overall health. It is a vital tool for diagnosing and managing diabetes, significantly reducing the risk of diabetes-related complications. Regular monitoring and working closely with healthcare providers can help individuals maintain healthy HbA1c levels and help minimize potential long-term complications of having elevated blood glucose levels.