In cardiology, specific blood tests are pivotal in diagnosing and assessing heart-related conditions. One such indispensable marker is troponin. In this article, we will delve into what troponin is, how it is performed, the circumstances where it is utilized, and its significance in identifying myocardial injury and diagnosing heart attacks.
What is Troponin?
Troponin is a protein in muscle tissue, particularly in the heart muscle (myocardium). It plays a crucial role in regulating muscle contraction. Troponin exists in three distinct forms – Troponin C, Troponin T, and Troponin I. However, when we refer to “troponin” in the context of cardiology, we are typically discussing Troponin T and Troponin I. When muscle tissue sustains an injury, troponin proteins are released into the bloodstream, allowing for their straightforward detection through a simple blood test.
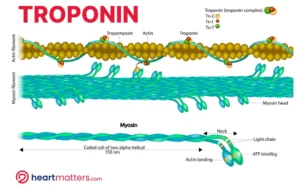
Illustration of a Muscle Fiber: Troponin, Actin, and Myosin Interaction. Troponin particles regulate muscle contraction by controlling the interaction between actin filaments (thin) and myosin filaments (thick). This regulatory process is crucial for muscle function and is a key component of the sliding filament theory of muscle contraction. When there is an injury to the muscle fiber, troponin particles are released and can be detected with a simple blood test.
How is Troponin Measured?
Troponin levels are measured via a blood test involving the collection of a blood sample from a patient’s vein, which is then sent to a laboratory for analysis. The laboratory employs specialized assays to detect and quantify Troponin T and Troponin I in the bloodstream. The greater the detected level of troponin in the blood typically corresponds to a more significant muscle injury.

Figure illustrating Troponin testing with a blood sample. A blood sample (depicted in a vial) is collected for troponin analysis, a diagnostic tool in cardiology. High-sensitivity troponin assays can detect even tiny troponin levels, enabling accurate assessment of cardiac health.
Circumstances for Troponin Testing
Troponin testing is primarily performed in the following circumstances:
- Chest Pain or Discomfort: When a patient presents with chest pain or discomfort, troponin testing is often employed to determine if there has been damage to the heart muscle, which can indicate a heart attack.
- Suspected Heart Attack: Troponin testing is integral to diagnosing a heart attack (myocardial infarction). Elevated levels of Troponin T or Troponin I in the blood indicate myocardial injury, a key diagnostic criterion for a heart attack.
- Monitoring Cardiac Patients: For patients with known heart conditions, troponin levels may be monitored over time to assess the status of the heart muscle and the effectiveness of treatments.
Troponin in the Diagnosis of Heart Attacks
When coronary arteries become blocked, depriving the heart muscle of oxygen, the heart muscle cells can be damaged. This damage releases troponin into the bloodstream. Elevated troponin levels in the context of chest pain or other symptoms consistent with a heart attack provide strong evidence for the diagnosis. There are, however, several other causes of troponin elevation, as shown below.
Causes of Troponin Elevation
Troponin, a vital cardiac biomarker, becomes elevated under different circumstances, often as a crucial indicator of heart and muscle health. This compilation outlines the diverse range of conditions that can contribute to elevated troponin levels, from cardiac events to medical conditions and external factors.
| Cause of Troponin Elevation | Description |
|---|---|
| 1. Myocardial Infarction (Heart Attack) | Damage to the heart muscle due to insufficient blood supply. |
| 2. Unstable Angina | Severe chest pain resulting from reduced blood flow to the heart. |
| 3. Arrhythmias, including Atrial Fibrillation (AF) | Rapid and irregular heart rhythms, such as AF, lead to troponin elevation when the heart is racing. |
| 4. Myocarditis | Heart muscle inflammation is often due to viral infections or autoimmune diseases. |
| 5. Pericarditis | Inflammation of the sac surrounding the heart (pericardium) can lead to troponin release. |
| 6. Cardiomyopathies | Various forms of heart muscle disease include hypertrophic or dilated cardiomyopathy. |
| 7. Pulmonary Embolism | Blood clots travel to the lungs, straining the right side of the heart and causing troponin release. |
| 8. Hypertensive Crisis | Extremely high blood pressure leads to an elevation of troponin due to increased heart strain. |
| 9. Cardiac Trauma | Injuries to the heart, such as blunt force trauma or cardiac surgery, cause troponin release. |
| 10. Takotsubo Cardiomyopathy (Broken Heart Syndrome) | Intense emotional or physical stress leads to temporary heart muscle weakening and troponin elevation. |
| 11. Drug-Induced Cardiotoxicity | Certain medications, including chemotherapy drugs, damage heart cells and cause troponin release. |
| 12. Chronic Kidney Disease | Kidney dysfunction elevates troponin as the kidneys clear troponin from the bloodstream. |
| 13. Sepsis | Severe infections impact heart function, leading to troponin release. |
| 14. Heatstroke | Severe overheating stresses the heart and causing troponin elevation. |
| 15. Electrolyte Imbalances | Disturbances in electrolyte levels, particularly potassium and calcium, affect heart muscle function and cause troponin release. |
| 16. Inflammatory Disorders | Certain autoimmune and inflammatory conditions lead to troponin elevation due to their impact on the heart. |
Conclusion
Troponin has emerged as an indispensable biomarker, particularly in evaluating patients presenting with chest pain. It is a valuable tool complementing clinical assessments and can indicate various conditions that stress the heart muscle. Typically performed in acute settings, such as emergency departments, troponin testing has become a cornerstone of cardiac evaluation. Its ability to provide critical insights into cardiac health underscores its importance in ensuring timely and accurate care for individuals seeking medical attention for cardiac concerns.