A heart attack is undoubtedly one of the most distressing complications that can cast a shadow over our hearts. However, I’ve realized that a seemingly simple calcium score can wield a similar power to disrupt lives. The news of an elevated calcium score has the potential to plunge individuals into a sea of unease and turmoil. Let’s delve deeper into the significance of this calcium score, aiming to restore some sense of calm as we navigate this territory together.
The calcium score, a well-established diagnostic tool validated by extensive long-term studies, can present unsettling results when it climbs higher. Due to their elevated score, many patients are informed of a specific percentage risk of developing cardiovascular issues such as a heart attack within the next decade. The weight of being told that their calcium score equates to a 10 to 20% risk of a heart attack is a burden that can hardly be ignored. The ensuing worry and stress can be all-encompassing.
Consider a high calcium score not as an end, but as a new chapter in your heart’s journey.
It’s indeed disheartening that many patients are in swift consultations with their healthcare providers, often receiving their test results with minimal explanation of the findings.
These interactions can be as brief as:
- Your calcium score is elevated.
- You face an increased risk of a heart attack.
- Here’s your prescription for statins.
Does this sound familiar to some of you?
This stripped-down approach often leaves individuals grappling with the weight of their results without a deeper comprehension of the implications or an opportunity to address their concerns.
This equation often lacks a comprehensive understanding of the calcium score and its implications. This informational void frequently drives patients to seek solace and clarity from online forums. My aspiration for this article is that it can help fill this informational gap and offer a beacon of understanding.
The Calcium Score: Explained
A calcium score measures calcified plaque in coronary arteries, which can narrow and block blood flow, leading to heart issues. A chest CT scan determines it via a non-invasive coronary artery calcium scoring test. The score predicts heart disease risk and guides prevention and treatment strategies.
Interpreting a High Calcium Score
A calcium score is measured in Agatston units, with higher scores indicating more calcified plaque. The scores are typically categorized into the following ranges:
- 0: No evidence of calcified plaque.
- 1-10: Minimal amount of plaque.
- 11-100: Mild plaque burden.
- 101-400: Moderate plaque burden.
- 400 and above: High plaque burden.
The calcium score is, in essence, a numerical representation generated through a diagnostic screening test. However, it alone cannot craft a complete decision-making strategy. Instead, we must holistically consider all cardiovascular risk factors and contextualize the score. Factors like age, the extent of calcium buildup, and the individual’s overall health landscape play pivotal roles in charting the path forward.
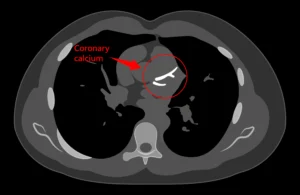
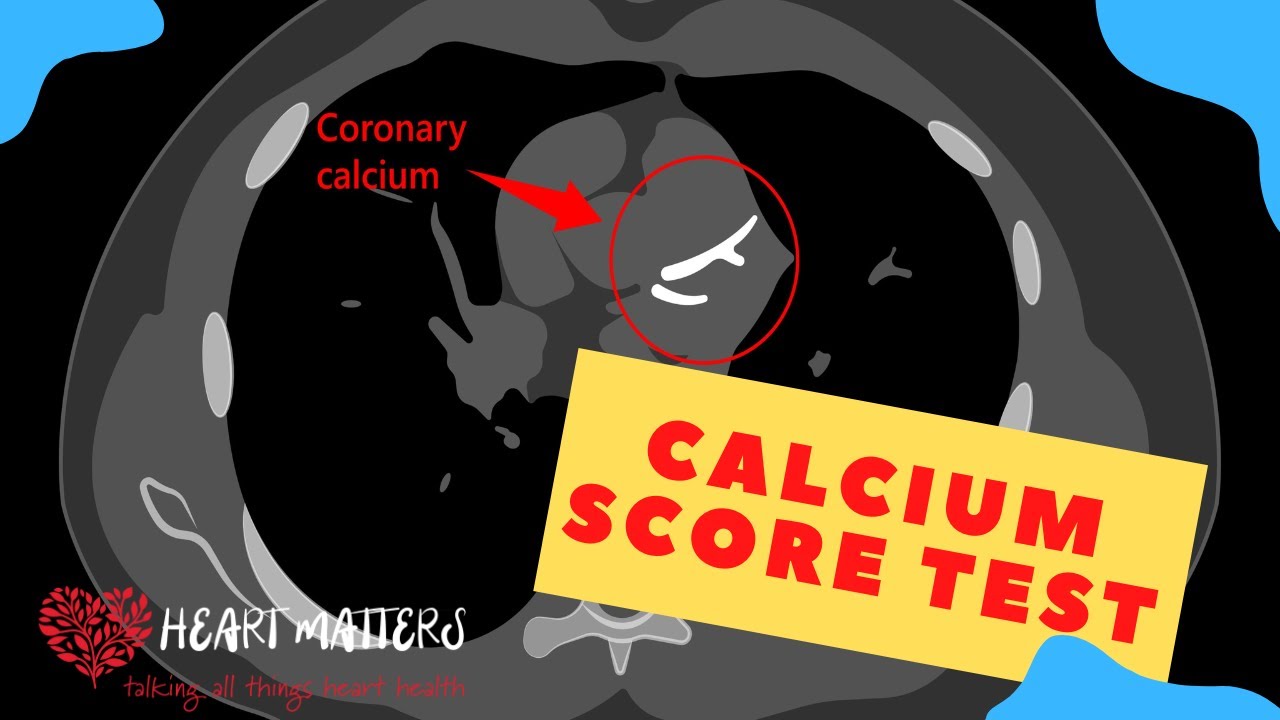
Picture the calcium score as an X-ray CT scan designed to spot calcium deposits around and within the heart’s arteries. Calcium, a foundational component of our bones, appears white on an X-ray due to its density. The CT scan methodically inspects the arteries, spotting the presence of this calcium material. Notably, a calcium score of 0 doesn’t guarantee an absence of lipid buildup within the heart’s arteries. An individual with a score of 0 might still have some lipid buildup.
Conversely, I’ve encountered patients with high calcium scores who undergo invasive angiograms only to find no substantial arterial narrowings. Conversely, individuals with previous calcium scores of 0 have later experienced heart attacks and severe blockages. This shows why it’s important to have a detailed understanding of the situation.
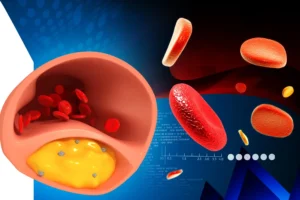
In the cross-section of the heart artery above, a yellow soft area denotes plaque, often without detectable calcium deposits when invasive imaging is performed. Therefore, while the calcium score does hint at calcium accumulation around arterial walls, it doesn’t inherently diagnose blockages within the arteries. A higher calcium score might suggest a heightened risk of internal plaque buildup, but this correlation isn’t absolute.
A high calcium score should never be misconstrued as a sentence of doom. Instead, it serves as a valuable signal, prompting proactive steps toward heart health.
Approach to the calcium score
I’ve had countless patients walk into my office, burdened by distress over their results. However, the calcium score is merely one piece of the puzzle. Our approach is to comprehensively assess your overall risk profile, considering all contributing factors. A high score signifies a need for more vigilant monitoring and an intensified effort to reduce risk factors. My practice involves meticulously reviewing medical histories and scrutinizing symptoms that might hint at reduced blood flow to the heart muscle, often called ischemic symptoms. These symptoms encompass chest discomfort, radiating pain in the arms, neck, jaw, or back, and shortness of breath during exertion.
Our evaluation extends to examining cardiac risks, including blood pressure, diabetes, smoking, and lifestyle choices. These factors, alongside additional tests, shape our endeavor to minimize long-term risks and foster an active life devoid of the shackles of fear.
A comprehensive blood panel, including a cholesterol profile assessment, guides our approach. For higher calcium scores, additional tests, such as assessing lipoprotein (a) levels, could reveal long-term risk markers.
Further examinations like stress tests or CT angiography might be warranted depending on symptoms. Collaborative efforts with dieticians can tackle raised cholesterol profiles and diabetes control. Medications could enter the picture if the calcium score is elevated to stabilize plaque and prevent rupture and subsequent heart attacks.
Remember, the treatment goal isn’t to reduce the calcium score; it’s about nurturing the stability of arterial plaque to avert potential calamity.
Through risk factor management and medications like aspirin and statins, we curtail cholesterol levels and combat inflammation within arterial walls. By diminishing inflammation, we enhance the strength and stability of arterial fibrous tissue, shielding against plaque instability and the resulting heart attacks. This strategy is effective, regardless of how high the calcium score is, and offers a path forward of positivity.
Remember, contrary to what one might assume, the primary aim isn’t merely to lower the calcium CT score. Instead, the focus is on minimizing the risks associated with calcium buildup. Medications, lifestyle modifications, and risk factor management are all part of the strategy. The goal is to stabilize any existing plaque, reducing the likelihood of it causing complications like heart attacks or strokes.
While a high calcium score might introduce anxiety, it’s crucial to acknowledge that it’s only a single element in the broader canvas of heart health. It is a window into cardiovascular health, offering valuable insights into potential risks. However, it’s essential to approach this score within the context of your broader health profile. Remember, it’s not a crystal ball that predicts your fate, but rather a tool that empowers healthcare professionals to guide you toward heart-healthy choices when combined with other information.

Conclusion
The journey forward is collaborative, exploring all facets of your health, understanding your unique risk profile, and crafting a strategy prioritizing stability and wellness. We can navigate these intricacies with dedication and guidance and empower you to lead a life free from the shackles of fear, driven by informed decisions and proactive health management. Your heart’s journey is complex but armed with knowledge, you can navigate it confidently and make informed decisions for a healthier future.