Our heart relies on a precise electrical system to maintain rhythm and function. This system works silently in the background most of the time, keeping our hearts beating steadily. However, sometimes, individuals may feel palpitations or irregular heartbeats. One potential cause of such palpitations is ventricular ectopics. In this article, we will explore ventricular ectopics, delving into what they are, how they may be assessed, and potential management strategies.
Understanding Ventricular Ectopics
Ventricular ectopics, sometimes called premature ventricular contractions (PVCs), are abnormal electrical impulses that originate in the heart’s ventricles, the lower chambers responsible for pumping blood to the rest of the body. These electrical signals disrupt the heart’s rhythm, leading to irregular heartbeats or palpitations.
Unlike the regular, coordinated beating of the heart, ventricular ectopics occur when the ventricles contract prematurely, out of sync with the heart’s natural electrical pattern. This can result in a sensation of the heart “skipping a beat” or a strong, forceful beat that follows a regular one.
Ventricular ectopics can affect individuals with or without underlying heart conditions. While they may be more common in those with heart issues, such as coronary artery disease or cardiomyopathy, they can also occur in otherwise healthy individuals. In some cases, they are harmless and do not require medical intervention. However, frequent or severe ventricular ectopics may warrant further evaluation by a healthcare professional to determine their underlying cause and potential management.
Stress and anxiety can release hormones like adrenaline, increasing the risk of ventricular ectopics. These ectopics can, in turn, worsen anxiety, forming a cycle. It’s important not to hastily link palpitations to anxiety or panic attacks. Instead, a comprehensive assessment is crucial for understanding and managing symptoms.
Causes and Triggers
Ventricular ectopics can have various underlying causes and triggers contributing to their occurrence. Understanding these factors is crucial in managing and potentially preventing these irregular heartbeats.
Stress and Anxiety
Elevated stress levels and anxiety can stimulate the release of stress hormones, such as adrenaline, which may increase the likelihood of ventricular ectopics. Managing stress through relaxation techniques and stress-reduction strategies can help mitigate this trigger.
Caffeine and Stimulants
Excessive consumption of caffeine, found in coffee, tea, energy drinks, and certain medications (e.g., salbutamol puffers for asthma), can stimulate the heart and potentially lead to ventricular ectopics. Reducing caffeine intake or avoiding it close to bedtime may help reduce the occurrence of these irregular beats.
Medications
Some medications, particularly those that affect the cardiovascular system, may increase the risk of ventricular ectopics. These can include certain antiarrhythmic drugs, decongestants, and over-the-counter cold or asthma medications like salbutamol puffers. If you suspect your medications contribute to ventricular ectopics, consult your healthcare provider for alternatives.
Electrolyte Imbalances
Abnormal levels of essential electrolytes like potassium, calcium, and magnesium can disrupt the electrical signals in the heart, potentially leading to ventricular ectopics. Maintaining a balanced diet and addressing any underlying medical conditions that affect electrolyte levels is essential.
Heart Conditions
Individuals with pre-existing heart conditions, such as coronary artery disease, heart failure, or cardiomyopathy, may be more prone to ventricular ectopics. Managing the underlying heart condition with appropriate medical care and lifestyle changes is essential in reducing their occurrence.
Alcohol and Substance Abuse
Excessive alcohol consumption and the use of certain recreational drugs can trigger irregular heartbeats, including ventricular ectopics. Limiting or avoiding these substances is vital for heart health.
Cigarette Smoking
Smoking has been associated with an increased risk of ventricular ectopics. Quitting smoking can reduce this risk and improve overall cardiovascular health.
Other Health Conditions
Some medical conditions, such as hyperthyroidism and chronic lung diseases, can indirectly affect the heart’s electrical system and contribute to ventricular ectopics. Iron deficiency can also trigger more ventricular ectopics and, therefore, palpitations. Proper management of these conditions is essential.
Hormonal changes
Hormonal changes, particularly during the menopausal phase, can increase the frequency and intensity of palpitations arising from ventricular ectopics. While such sensations are generally harmless, seeking guidance from a healthcare professional is recommended to exclude any underlying concerns.
By understanding the potential causes and triggers of ventricular ectopics, individuals can take proactive steps to reduce their occurrence. When necessary, lifestyle modifications, stress management, and medical consultation are key elements in managing these ectopic heartbeats.
Assessment and Diagnosis
Accurately diagnosing ventricular ectopics is crucial to determine their cause and appropriate management. The diagnostic process often involves a combination of clinical evaluation and medical tests.
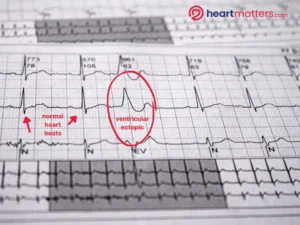
This ECG shows normal heartbeats alongside an ectopic heartbeat. The ectopic beat is broader and more prominent because it originates from a different part of the heart. It causes a wider QRS interval on the ECG.
Keep in mind that not all individuals with ventricular ectopics require treatment, and management strategies vary based on the underlying cause and symptom severity.
Clinical Evaluation
The initial step in diagnosing ventricular ectopics is a thorough clinical evaluation. Your healthcare provider will take a detailed medical history, paying close attention to any family history of heart conditions. They will inquire about the nature of your symptoms, such as palpitations, irregular heartbeats, or discomfort. The frequency and duration of these symptoms are essential information. Additionally, reporting these episodes is crucial if you’ve experienced presyncope (near-fainting) or syncope (fainting).
Physical Examination
A physical examination allows your healthcare provider to assess your overall health and gather clues about the underlying cause of ventricular ectopics. They will listen to your heart and lungs, check your blood pressure, and examine for signs of other medical conditions.
Electrocardiogram (ECG or EKG)
An ECG is a fundamental test for diagnosing ventricular ectopics. More details can be found here. It records the electrical activity of your heart and can detect irregular heartbeats, including premature ventricular contractions (PVCs). It provides valuable information about the timing and origin of these irregular beats.
Holter Monitor
For individuals with infrequent symptoms, a Holter monitor may be recommended. This portable device continuously records your heart’s electrical activity over 24 to 48 hours, allowing healthcare professionals to capture and analyze irregular heartbeats. More details on the Holter monitor are in our article linked here.
Event Monitor
Like a Holter monitor, an event monitor is worn for extended periods, often weeks to months. It is typically used for patients with sporadic symptoms. When you experience symptoms, you can activate the monitor to record your heart’s activity during that specific time.
Echocardiogram
An echocardiogram is an ultrasound of the heart that provides detailed images of its structure and function. It helps rule out underlying structural heart diseases that may contribute to ventricular ectopics. More details here.
Blood Tests
Blood tests may be conducted to assess the levels of electrolytes, such as potassium, calcium, and magnesium, as imbalances in these minerals can trigger irregular heartbeats. Your healthcare provider may also check thyroid hormone levels, as thyroid disorders can affect heart rhythm. A check of iron levels may also be worthwhile in some individuals as iron deficiency can trigger more ectopics and, therefore, palpitations.
Medication Review
Your doctor will review your current medications, as some can influence heart rhythms. This includes medications for asthma, where drugs like salbutamol puffers can impact heart rhythm.
Exercise Stress Test
In some cases, an exercise stress test may be recommended to evaluate how your heart responds to physical activity. This test can help identify exercise-induced ventricular ectopics.
Electrophysiological Studies (EPS)
EPS may be performed in complex cases or when ventricular ectopics are frequent and symptomatic. It involves the insertion of catheters into the heart to measure electrical activity and identify the source of irregular beats.
Cardiac MRI or CT Scan
These imaging studies may be utilized to assess the heart’s structure and function in more detail, especially if structural abnormalities are suspected.
The combination of clinical evaluation and these tests allows healthcare professionals to determine the cause and severity of ventricular ectopics and develop an appropriate treatment plan. Not all individuals with ventricular ectopics require treatment, and management strategies vary based on the underlying cause and symptom severity. Your healthcare provider will work closely with you to determine the best action.
Reassurance, following a thorough clinical assessment and initial investigations, plays a crucial role in confirming the benign nature of these symptoms. Confirming that the heart functions normally and highlighting that these symptoms frequently resolve without intervention offers considerable comfort and peace of mind to those experiencing these ectopics.
Management and Treatment
Addressing ventricular ectopics involves a multifaceted approach that aims to reduce the frequency and discomfort of these irregular heartbeats. Depending on the severity and underlying causes, various management strategies can be employed to improve the overall quality of life for individuals experiencing ventricular ectopics.
Lifestyle Changes
-
- Dietary Modifications: Adjusting your diet to include heart-healthy foods and reduce or eliminate triggers such as caffeine or alcohol.
- Avoidance of Triggering Factors: Identifying specific triggers, such as stress or certain foods, and taking steps to avoid or minimize exposure to them. Keeping hydrated is also key for overall health and wellness.
- Exercise and Physical Activity: Incorporating regular physical activity into your routine, as exercise can have a positive impact on heart health.
Stress Reduction Techniques
-
- Relaxation Techniques: Learning and practicing relaxation methods like deep breathing, progressive muscle relaxation, or guided imagery.
- Mindfulness and Meditation: Engaging in mindfulness practices and meditation to reduce stress and anxiety.
- Counseling and Support: Seeking the guidance of a mental health professional or support groups to address underlying stress or anxiety issues.
Medication
-
- Medications to Manage Underlying Conditions: If ventricular ectopics are related to an underlying condition like hypertension or thyroid disorders, medications to control these conditions may be recommended.
- Anti-arrhythmic Medications: Depending on the severity and frequency of ventricular ectopics, your healthcare provider may prescribe anti-arrhythmic medications to regulate heart rhythm.
- Medication for Anxiety or Stress (if applicable): In cases where anxiety or stress is a significant trigger, medications to manage these emotions may be considered.
Conclusion
Ventricular ectopics are common, often causing palpitations. It’s important to recognize that, in many cases, these ectopics are benign and require nothing more than simple reassurance. However, a comprehensive assessment by a healthcare professional is essential to rule out any underlying issues and confirm the harmless nature of these symptoms. This reassurance and guidance give individuals peace of mind and the confidence to manage these heart irregularities effectively.


