Supraventricular tachycardia, or SVT for short, is a type of heart arrhythmia that can cause an abnormally fast heart rate. The condition arises from the heart’s upper chambers, with heart rates usually between 150 and 220 beats per minute. This article will explore what SVT is, its causes, symptoms, diagnosis, and treatment options.
What is Supraventricular Tachycardia (SVT)?
SVT is a type of heart arrhythmia that occurs when an abnormal electrical impulse occurs in the heart’s upper chambers (atria). This results in a rapid heart rate ranging from 150 to 220 beats per minute. While SVT is not generally life-threatening, it can be uncomfortable and cause symptoms.
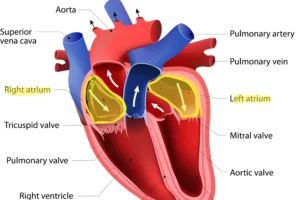
The atria are the two top chambers of the heart, highlighted in yellow. Supraventricular tachycardia arises from these areas of the heart, causing the heart to beat fast at rates between 150-220 beats per minute.
Types of supraventricular tachycardia (SVT)
While the precise cause of SVT remains unclear, various factors are believed to contribute to its development, primarily involving abnormalities in the heart’s electrical pathways. Simplifying the concept, SVT occurs when additional areas of the heart’s electrical system activate, initiating extra circuits that prompt rapid heart rates.
These circuits/pathways include:
1. Atrioventricular Nodal Reentrant Tachycardia (AVNRT):
- AVNRT is the most prevalent form of supraventricular tachycardia.
- It occurs when an abnormal electrical pathway within the heart’s atrioventricular (AV) node is a crucial part of the electrical conduction system. Think of it as a misfired electrical circuit.
- During AVNRT, electrical signals within the heart re-enter the AV node, leading to rapid and irregular heartbeats.
- This type of SVT can affect individuals of various age groups.
2. Atrioventricular Reciprocating Tachycardia (AVRT):
AVRT, the second most prevalent subtype of supraventricular tachycardia, exhibits a higher incidence among younger demographics. This form frequently entails the presence of an accessory pathway, termed the Kent bundle, which facilitates the diversion of electrical signals away from the heart’s usual conduction system. Consequently, AVRT can induce swift and irregular heart rhythms, which are attributed to the abnormal circuitry within the heart. Notably, palpitations are a common manifestation of AVRT, and in some instances, more severe symptoms may ensue.
3. Atrial Tachycardias:
These episodes typically originate from a distinct part of the heart’s electrical circuitry. Among the frequently observed conditions are atrial fibrillation and atrial flutter. Atrial tachycardias encompass a spectrum of arrhythmias, including focal atrial tachycardias and multifocal atrial tachycardias, each characterized by unique mechanisms and clinical features. Common triggers for these tachycardias include structural heart disease, electrolyte imbalances, and pulmonary disorders. Symptoms can vary from palpitations and chest discomfort to more serious manifestations like dizziness and syncope.
Triggers of supraventricular tachycardia
1. Structural Heart Defects:
Structural abnormalities within the heart, such as congenital heart defects, valve disorders, or muscle disorders (cardiomyopathies), can disrupt the heart’s electrical pathways, leading to SVT. These defects may create abnormal circuits or pathways that facilitate the rapid generation and propagation of electrical impulses, contributing to tachycardic episodes.
2. Certain Medications:
Certain medications, particularly those that affect the heart’s electrical activity or alter its autonomic regulation, can trigger or exacerbate SVT.
3. Stimulants such as Caffeine or Nicotine:
Stimulants like caffeine, found in coffee, tea, energy drinks, and certain medications, can stimulate the heart and nervous system, potentially triggering SVT in susceptible individuals. Similarly, nicotine, present in tobacco products such as cigarettes and electronic cigarettes, can exert stimulatory effects on the heart, increasing the likelihood of tachycardic episodes.
4. Emotional Stress or Anxiety:
Emotional stress and anxiety can have profound effects on the cardiovascular system, including alterations in heart rate and rhythm. Elevated levels of stress hormones, such as adrenaline and cortisol, can stimulate the heart and exacerbate sympathetic nervous system activity, leading to episodes of SVT in some individuals.
5. Heavy Alcohol Use:
Excessive alcohol consumption can disrupt the normal electrical activity of the heart, predisposing individuals to arrhythmias like SVT. Alcohol-induced changes in electrolyte balance, autonomic tone, and myocardial function can contribute to the development of tachycardic episodes, particularly in individuals with underlying susceptibility factors.
Symptoms of SVT
The symptoms of SVT can vary from person to person and may come and go. Some individuals may experience no symptoms at all. Common symptoms of SVT include:
- Rapid heartbeat
- Palpitations (a fluttering or pounding sensation in the chest)
- Chest discomfort or pain
- Shortness of breath
- Dizziness or lightheadedness
- Fainting or near fainting
- Fatigue

Diagnosis of supraventricular tachycardia (SVT)
Diagnosis of SVT typically involves a physical examination, medical history, and various tests. These may include:
- Electrocardiogram (ECG): This test records the heart’s electrical activity and can help identify abnormal rhythms.
- Holter monitor: This portable device records the heart’s activity over 24 hours and can help detect abnormal rhythms that may not appear on a regular ECG.
- Echocardiogram: This test uses sound waves to create heart images and can help identify structural abnormalities.
- Electrophysiology study: This invasive procedure involves inserting small wires into the heart to evaluate the heart’s electrical system and identify abnormal pathways.
If feasible, I advise my patients to promptly undergo an electrocardiogram or seek assistance from paramedics if they have concerns. Paramedics can perform a heart tracing to aid in diagnosing SVT.
Treatment of supraventricular tachycardia (SVT)
The treatment of SVT depends on the severity and frequency of symptoms. Treatment options for SVT may include:
- Vagal maneuvers, including holding one’s breath, coughing, or bearing down as if having a bowel movement, can effectively slow the heart rate. One technique I often recommend to patients is akin to equalizing ear pressure while flying—an action of bearing down on a pinched nose can yield similar results.
- Medications: Certain medications, such as beta-blockers or calcium channel blockers, can help slow the heart rate and prevent episodes of SVT.
- Cardioversion: This procedure involves using electrical shock to reset the heart’s rhythm back to normal.
- Catheter ablation: This minimally invasive procedure involves inserting a catheter into the heart and using radiofrequency energy to destroy the abnormal pathway causing the SVT.
Prevention of supraventricular tachycardia (SVT)
While SVT may not always be preventable, there are some steps individuals can take to reduce their risk of developing the condition. These include:
- Avoiding triggers, such as stimulants or emotional stress
- Managing underlying medical conditions, such as high blood pressure or thyroid disorders
- Maintaining a healthy lifestyle, including regular exercise and a balanced diet
- Quitting smoking or limiting alcohol consumption
Conclusion
SVT is a common type of heart arrhythmia that can cause uncomfortable symptoms such as rapid heartbeat, chest discomfort, and shortness of breath. While the condition is typically not life-threatening, it can be managed with proper medical care and treatment. If you experience any symptoms of SVT, it is important to speak with a healthcare provider to receive appropriate evaluation and management.