The heart’s intricate network of electrical pathways governs the rhythm that sustains our body’s functioning. Yet, disruptions can occur, giving rise to abnormal heart rhythms or arrhythmias. One of these is ventricular tachycardia (VT), a condition with potentially significant implications for cardiovascular well-being. This article examines ventricular tachycardia, encompassing its origins, symptoms, diagnosis, and some of the potential treatment considerations.
Understanding Ventricular Tachycardia (VT)
Ventricular tachycardia is a rapid heart rhythm originating from the ventricles, the lower chambers of the heart responsible for pumping oxygenated blood to the rest of the body. In VT, the ventricles beat abnormally fast, exceeding 100 beats per minute, and more often greater than 150bpm. This abnormal rhythm disrupts the heart’s pumping action, potentially leading to decreased blood flow and compromising organ function. See below illustrative animation demonstrating the electrical stimuli arising from the lower chambers of the heart.
Causes of Ventricular Tachycardia
Various factors can influence ventricular tachycardia’s development and predispose individuals. Common associations include structural heart diseases (like coronary artery disease, heart attacks, cardiomyopathy, and heart valve abnormalities), as well as genetic conditions, electrolyte imbalances, drug interactions, and prior heart surgeries. During diagnosis, it’s crucial to carefully assess these potential causes, including any underlying conditions or risk-raising factors.
Importantly, VT’s causes are often multifaceted, with individual cases influenced by a combination of these factors. Swift diagnosis and management are vital for effectively addressing both VT and its underlying triggers.
A summary of some causes that need to be considered:
- Coronary Artery Disease: Narrowed or blocked coronary arteries can disrupt blood flow to the heart muscle, leading to abnormal electrical impulses that trigger VT.
- Heart Attack (Myocardial Infarction): The damage to the heart muscle caused by a heart attack can create a substrate for VT to develop.
- Cardiomyopathy: Conditions such as dilated cardiomyopathy or hypertrophic cardiomyopathy can lead to structural changes in the heart that increase the risk of VT.
- Heart Failure: A weakened heart muscle and impaired pumping function can create an environment conducive to VT.
- Electrolyte Imbalances: Abnormal levels of potassium, magnesium, or other electrolytes can disrupt the heart’s electrical signals and trigger VT.
- Long QT Syndrome: Inherited genetic disorders that affect the heart’s electrical system can lead to irregular heartbeats, including VT. More details here.
- Brugada Syndrome: Another inherited genetic disorder that can cause abnormal heart rhythms, including VT.
- Drug Side Effects: Certain medications, especially those that affect the heart’s electrical conduction, can increase the risk of VT.
- Stimulant Abuse: Excessive consumption of stimulants or illicit drugs can trigger abnormal heart rhythms, including VT.
- Scar Tissue from Prior Heart Surgery: Surgical procedures can lead to scar tissue formation that disrupts normal electrical pathways, increasing the risk of VT.
- Inflammatory Conditions: Conditions like myocarditis (inflammation of the heart muscle) can lead to VT.
- Certain Genetic Mutations: Specific genetic mutations can make individuals more susceptible to developing VT.
- Acute Illness or Stress: Severe illness or intense physical or emotional stress can sometimes trigger VT, especially in individuals with underlying heart conditions.
- Abnormal Heart Valves: Conditions like mitral valve prolapse can lead to VT in some cases.
Recognizing the Symptoms
The symptoms of ventricular tachycardia can vary depending on the severity and duration of the episodes. Some individuals may remain asymptomatic, while others may experience palpitations, rapid and irregular pulse, lightheadedness, dizziness, chest pain, shortness of breath, fainting, or even cardiac arrest. It is crucial to seek medical attention if any of these symptoms are experienced.
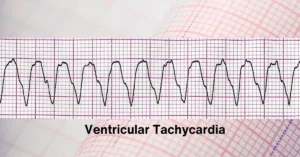 This ECG depicts a clear example of monomorphic ventricular tachycardia (VT) characterized by a consistent QRS morphology and a rapid heart rate. The distinctive feature of monomorphic VT is the uniform appearance of QRS complexes on the ECG, reflecting a single origin of the arrhythmia. The rapid ventricular rate is indicative of the sustained nature of this tachycardia
This ECG depicts a clear example of monomorphic ventricular tachycardia (VT) characterized by a consistent QRS morphology and a rapid heart rate. The distinctive feature of monomorphic VT is the uniform appearance of QRS complexes on the ECG, reflecting a single origin of the arrhythmia. The rapid ventricular rate is indicative of the sustained nature of this tachycardia
Diagnosing Ventricular Tachycardia
Prompt and precise diagnosis of ventricular tachycardia is vital for effective management. The diagnostic process is multifaceted, beginning with a thorough review of the patient’s medical history and a comprehensive physical examination. These initial steps lay the foundation for further diagnostic assessments, which encompass:
- Electrocardiograms (ECGs or EKGs): These play an important role in identifying VT episodes and possible origins by recording the heart’s electrical activity.
- Heart monitors / event monitors: These devices allow continuous monitoring to capture any irregularities that might not show up during short-term ECGs.
- Echocardiography: This imaging technique utilizes sound waves to create detailed images of the heart’s structure and function, aiding in identifying any structural abnormalities.
- Stress tests: By observing the heart’s response to physical exertion, stress tests provide valuable information about its functionality and potential triggers for VT.
- Cardiac MRI: This advanced imaging technology provides highly detailed images of the heart, aiding in the assessment of its structure and identifying potential causes of VT.
- Electrophysiological studies: These studies involve detailed mapping of the heart’s electrical pathways and may be conducted to precisely identify the origins of VT and assess the condition’s severity.
Together, these assessments help medical professionals gain a comprehensive understanding of the underlying causes and characteristics of ventricular tachycardia, enabling informed decisions about management and treatment strategies.
Cardiac MRI offers a non-invasive way to visualize the heart’s structure, identify underlying structural abnormalities, and accurately locate the origin of the tachycardia. By providing detailed insights into myocardial tissue, scar tissue, and overall cardiac function, cardiac MRI plays a crucial role in guiding treatment strategies and improving the management of VT patients.
Treatment Options for Ventricular Tachycardia
Ventricular tachycardia is typically addressed by specialized cardiologists who have undergone sub-specialty training in the heart’s electrical/conduction system and the management of arrhythmias. Therefore, it may not be uncommon for your cardiologist to refer you to a colleague with this expertise.
The management of ventricular tachycardia aims to prevent life-threatening complications and restore normal heart rhythm. The treatment strategy depends on several factors, including the severity of symptoms, underlying causes, and associated risks. Options range from medication to medical devices and invasive procedures.
- Medications: Antiarrhythmic drugs are often prescribed to control ventricular tachycardia episodes. Medications like beta-blockers, calcium channel blockers, and sodium channel blockers work by regulating the electrical impulses in the heart.
- Implantable Cardioverter-Defibrillator (ICD): For some individuals who are assessed as having a high risk of cardiac arrest or recurrent VT episodes, an ICD may be implanted. This device continuously monitors the heart’s rhythm and delivers a shock internally to restore normal rhythm if a dangerous arrhythmia is detected.
- Catheter Ablation: In certain cases, catheter ablation may be recommended. This minimally invasive procedure involves the insertion of a catheter into the heart to destroy the abnormal electrical pathways causing VT.
- Acute Cardiac Defibrillation: In situations where ventricular tachycardia persists and poses a threat to vital functions, such as blood pressure, immediate intervention becomes necessary. In these cases, a cardiac defibrillator may be utilized to perform cardioversion, a process that involves delivering a controlled electric shock to the chest. This procedure aims to restore a normal heart rhythm and overcome the irregularities associated with ventricular tachycardia.
Preventive Measures
While ventricular tachycardia can be a serious condition, there are steps individuals can take to reduce the risk of developing or worsening the condition. Lifestyle modifications such:
- Embracing a Heart-Healthy Lifestyle: We keep returning to this message often in our heart health articles. Incorporating a heart-healthy lifestyle can have a profound impact on overall outcomes when it comes to cardiovascular disease. By paying careful attention to underlying risk factors, you can optimize long-term results. Prioritizing regular exercise, maintaining a healthy weight, abstaining from tobacco products, and practicing moderate alcohol consumption are all crucial components for promoting cardiovascular well-being.
- Medication Compliance: If prescribed antiarrhythmic medications, it is crucial to take them as directed by the healthcare provider. Skipping doses or abruptly stopping medication can increase the risk of rhythm disorders. It is important to communicate with the healthcare team regarding any concerns or side effects experienced.
- Effective Management of Underlying Conditions: Ensuring proper management of underlying heart conditions, including coronary artery disease, cardiomyopathy, or heart valve disorders, plays a pivotal role in preventing ventricular tachycardia. Regular check-ups, diligent adherence to treatment plans, and following healthcare recommendations are essential for maintaining optimal heart health. Collaborating closely with local healthcare professionals ensures your condition is diligently monitored, empowering you to lead a fulfilling life to the fullest extent.
- Regular Follow-up and Monitoring: Routine follow-up appointments with healthcare providers are essential for monitoring the condition and adjusting treatment plans if necessary. Regular check-ups allow for ongoing evaluation of the heart’s function, assessment of medication effectiveness, and detection of any changes in symptoms.
Conclusion
Ventricular tachycardia is a heart rhythm disorder that requires a comprehensive understanding, timely diagnosis, and proper management. By recognizing the symptoms, seeking prompt medical attention, and following recommended treatment strategies, individuals can minimize the risks associated with VT and enhance their quality of life. Additionally, adopting a heart-healthy lifestyle, effectively managing underlying conditions, adhering to prescribed medications, avoiding triggers, and maintaining regular follow-up appointments can greatly reduce the likelihood of VT episodes and potential complications. Remember, when it comes to matters of the heart, knowledge, and proactive care are vital for a healthier and more informed future.


