Digoxin is a medication utilized for various heart conditions. With a history dating back centuries, it remains a significant treatment for heart failure, atrial fibrillation, and related issues. This article delves into the intricacies of digoxin, providing insights into its functions, advantages, and potential drawbacks. Discover how it operates, its administration, and precautions for its safe usage.
Mechanism and Uses
Digoxin boosts heart muscle contractions and regulates rhythm. Inhibiting the sodium-potassium pump increases intracellular calcium levels, improving myocardial contraction (pumping strength). It also slows heart rate and controls certain arrhythmias like atrial fibrillation.
Trade names
Several variations/names of digoxin are branded around the world. Some are shown below:
- Lanoxin
- Digitek
- Lanoxicaps
- Toloxin
- Cardoxin
- Digacin
- Digobal
Indications and Benefits
Primarily used to treat congestive heart failure, it improves heart function and alleviates symptoms. Effective in atrial fibrillation and flutter, it can enhance quality of life and decrease hospitalizations. Additionally, it reduces stroke risk and sudden death in specific heart failure cases.
Potential Risks
While generally safe, potential risks include toxicity due to excessive dosing. People with certain medical conditions, like kidney or liver disease, are more susceptible to toxicity.
Side Effects of Digoxin:
- Nausea
- Vomiting
- Headache
- Dizziness
- Irregular heartbeat (Seek immediate medical attention)
- Vision changes (Seek prompt medical attention)
- Confusion (Seek prompt medical attention)
Precautions for Taking Digoxin:
- Follow your healthcare provider’s instructions carefully, including the prescribed dosage.
- Attend regular check-ups to monitor heart function and medication levels.
- Inform your healthcare provider about your medications and supplements to avoid potential interactions.
- Maintain a consistent potassium level in your diet, as low potassium levels can increase the risk of side effects.
Taking digoxin under the guidance of a healthcare professional and staying vigilant about potential side effects and drug interactions is crucial for its safe and effective use.
In clinical practice, it is not uncommon to encounter nonspecific symptoms that may be attributed to digoxin use, especially in the elderly population. In such cases, a prudent approach often involves considering alternative treatment options or utilizing the lowest effective dose, recognizing that these nonspecific symptoms can significantly impact the quality of life.
Monitoring and Dosage
Although digoxin is generally considered safe and effective, there are potential risks associated with its use. These include an increased risk of toxicity if the dose is too high. In addition, people with certain medical conditions, such as kidney or liver disease, may be at increased risk of toxicity. Talking to your doctor about potential risks before taking digoxin is important. Regular monitoring of digoxin levels is crucial to avoid toxicity. Dosage adjustments are often based on renal function and age, as the drug is eliminated primarily by the kidneys. Closely monitoring electrolyte levels, especially potassium, is essential to ensure digoxin’s effectiveness and safety.

Dosing and Administration: How to Take Digoxin
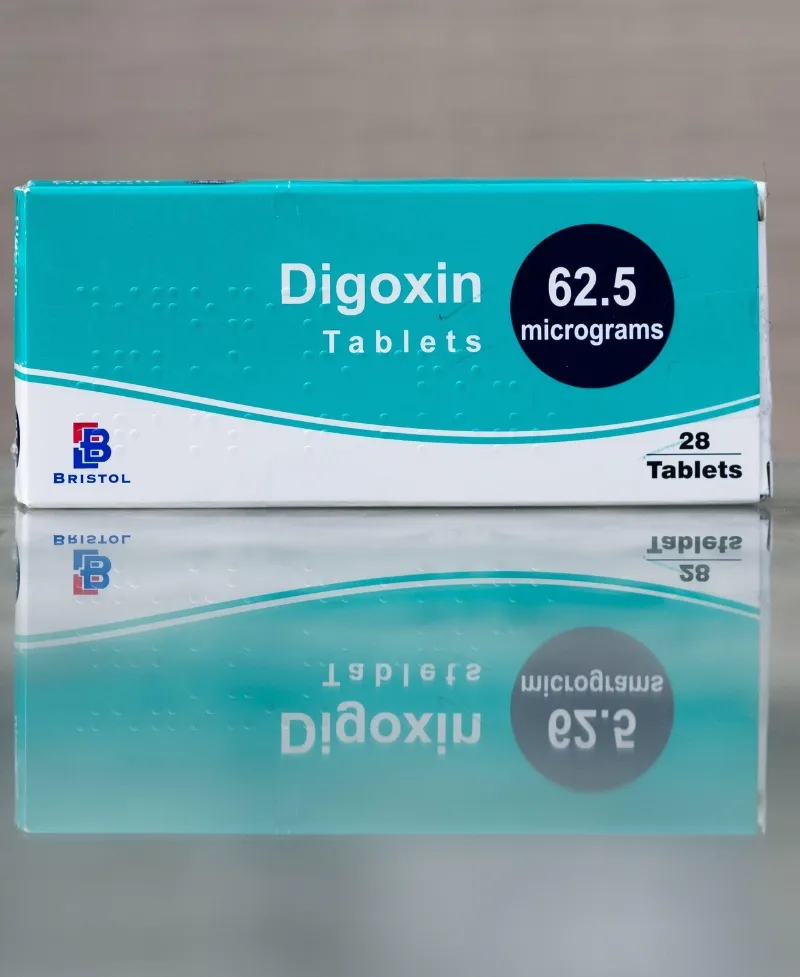
Oral Digoxin
Digoxin is available in oral form, usually as tablets or elixirs. Your healthcare provider will determine the appropriate dosage based on age, kidney function, and the treatment condition. Following their instructions meticulously is crucial to ensure safe and effective usage.
Dosage Initiation
The initiation of digoxin often involves a loading dose, where a higher initial dose is administered to achieve therapeutic levels in the bloodstream. Subsequent doses are then adjusted to maintain these levels.
Maintenance Dosing
Once therapeutic levels are achieved, maintenance doses are typically lower than the loading dose. They aim to sustain the desired therapeutic effect while minimizing the risk of side effects.
Monitoring
Regular monitoring of digoxin levels is essential to avoid toxicity. Blood tests will measure the concentration of digoxin in your bloodstream. These tests guide dose adjustments and ensure your levels remain within the therapeutic range.
IV Digoxin Use
In some instances, intravenous (IV) administration of digoxin may be necessary. IV digoxin is often used in hospital settings for acute management of heart conditions, particularly when rapid response is required.
Special Considerations
Elderly patients and those with impaired kidney function may require lower doses to prevent toxicity. Kidney function plays a significant role in digoxin elimination, so adjustments are crucial for patients with reduced kidney function.
Digibind (Digoxin-specific antibody fragments) is a medication used as an antidote for digoxin toxicity. When digoxin levels become dangerously high and lead to toxicity, Digibind works by binding to the excess digoxin in the body, effectively neutralizing its effects. This can be a critical intervention in cases of severe digoxin overdose or when toxicity occurs due to various factors. By helping to remove the excess digoxin, Digibind helps to restore a safer balance and prevent further harm. It’s important to administer Digibind under the supervision of healthcare professionals in cases of suspected digoxin toxicity.

Role in Cardiac Health
Digoxin exerts its therapeutic effects by interacting with the heart’s electrical and mechanical functions. It belongs to a class of drugs known as cardiac glycosides, with a primary target of the sodium-potassium ATPase pump, a vital enzyme found in heart cells.
Enhancing Heart Contraction
Digoxin’s foremost action is to increase the force of heart contractions. It does this by inhibiting the sodium-potassium pump, accumulating sodium inside heart cells. This sodium buildup alters the concentration gradient and indirectly promotes an influx of calcium into the cells. Calcium is essential for muscle contraction, so the increased intracellular calcium levels result in more forceful heart contractions.
Regulating Heart Rate
Additionally, digoxin influences the electrical activity of the heart. It slows down the rate at which electrical signals travel through the atrioventricular (AV) node, which helps to control the heart rate. Digoxin can be particularly effective in controlling heart rate in conditions like atrial fibrillation by delaying the passage of signals.
Balancing Fluid Levels
Digoxin’s effects extend beyond the heart. It can also impact the kidneys by promoting increased urine production and reducing fluid retention. This contributes to alleviating symptoms of congestive heart failure, such as swelling and shortness of breath.
Potential Challenges
While digoxin’s mechanism of action offers valuable therapeutic benefits, its narrow therapeutic window requires careful monitoring to prevent toxicity. High blood digoxin levels can adversely affect the heart and other organs.
Modern Role
Digoxin remains valuable in the current cardiology era, particularly in managing heart failure and specific arrhythmias. However, its use has become more selective due to the availability of alternative medications and interventions. Along with other heart failure treatments and antiarrhythmics, digoxin can improve a patient’s quality of life and symptom management.
Conclusion
Digoxin has an enduring legacy in cardiovascular medicine. Its potential to enhance heart function and regulate rhythm has secured its role in cardiac treatments. When prescribed cautiously, closely monitored, and integrated with comprehensive care, digoxin remains valuable for managing heart failure and arrhythmias. Consult healthcare professionals for personalized guidance on its usage, considering individual medical needs.