You may be familiar with the terms “bad cholesterol” (LDL) and “good cholesterol” (HDL). Doctors are beginning to understand that the story is even more complicated than this. We now understand that specific types of cholesterol-carrying particles (lipoproteins) affect the risk of stroke and heart attack. One of these particles is called lipoprotein(a). This article summarizes what we know about lipoprotein(a) and cardiovascular risk, when to test for it, and what we should do about high levels.
What are Lipoproteins
Cholesterol and triglycerides are lipids (fats). Unlike proteins, they are not water-soluble. The body packages lipids with proteins to make them soluble in the blood to transport them into the bloodstream. These microscopic transport particles are called lipoproteins. Cholesterol enters the body from the diet via the intestine and is also manufactured in the liver.
The body needs cholesterol to make cell membranes and certain hormones. Different lipoproteins transport lipids from the small intestine (i.e. from dietary intake) to the liver, from the liver to the peripheral tissues to be utilized, and from the peripheral tissues back to the liver to be degraded.
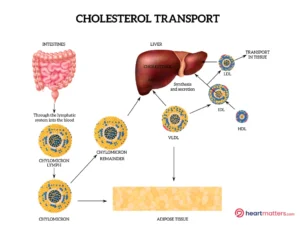
The primary types of lipoproteins of clinical relevance are:
Low-Density Lipoprotein (LDL): Often referred to as “bad” cholesterol, high levels of LDL can lead to cholesterol buildup in arteries, increasing the risk of heart disease.
High-Density Lipoprotein (HDL): Termed “good” cholesterol, HDL helps remove excess cholesterol from the bloodstream, reducing the risk of arterial plaque formation.
Very Low-Density Lipoprotein (VLDL): VLDL carries triglycerides and cholesterol from the liver to cells throughout the body. As VLDL particles release triglycerides, they become LDL particles, contributing to artery plaque formation if present in excess.
Lipoprotein(a) – The Lesser-Known Player: Lp(a) is a unique lipoprotein that consists of an LDL-like particle linked to a protein called apolipoprotein(a). While its exact function is still being studied, elevated Lp(a) levels have been associated with an increased risk of atherosclerosis, heart attacks, and strokes.
Emerging Evidence of Cardiovascular Risk
Recent research has underscored the significance of Lp(a) in cardiovascular health. High levels of Lp(a) appear to contribute to the narrowing of arteries, thrombosis (blood clot formation), and inflammation, all of which are key factors in cardiovascular disease.
High levels of Lp(a) in the blood have been associated with an increased risk of heart disease, stroke, and peripheral artery disease. Lp(a) can contribute to the development of atherosclerosis, which is the buildup of plaque in the arteries. This can lead to blockages and reduce blood flow to the heart and other organs, increasing the risk of heart attack and stroke.
Lp(a) levels are primarily determined by genetics, meaning some people are likelier to have higher Lp(a) levels than others. However, lifestyle factors like diet, exercise, and smoking can influence Lp(a) levels.
How can Lp(a) levels be measured?
Lp(a) levels can be measured with a blood test. However, it is important to note that Lp(a) levels can vary widely depending on the laboratory that performs the test. In addition, Lp(a) levels do not respond to lifestyle changes or medications like other types of cholesterol do.
When to Consider Lp(a) Testing
Lp(a) testing may be considered under the following circumstances:
Family History:
Individuals with a family history of premature cardiovascular disease may have a genetic predisposition to elevated Lp(a) levels.
Unexplained Heart Disease:
If someone experiences heart disease at a young age or without traditional risk factors, Lp(a) testing could offer insights.
Recurrent Cardiovascular Events:
For those who continue to experience cardiovascular events despite standard treatments, Lp(a) levels could provide additional diagnostic information.
Treatment Strategies
No medication is specifically approved to lower Lp(a) levels. However, some medications that lower LDL cholesterol may also moderately affect Lp(a) levels. These include statins, niacin, and PCSK9 inhibitors. In addition, lifestyle changes such as eating a healthy diet, exercising regularly, maintaining a healthy weight, and quitting smoking may help lower Lp(a) levels to some extent. However, these lifestyle changes may have a smaller effect on Lp(a) levels than other cholesterol types.
Lifestyle modifications:
There is a strong genetic predisposition to high lipoprotein levels (a). Lifestyle changes have only a minimal effect on lipoprotein(a) levels. However, the risk of heart attack and stroke is multifactorial, and instituting a healthy lifestyle (maintaining a heart-healthy diet, regular exercise, and avoiding smoking) will reduce overall cardiovascular risk significantly.
Medications:
Niacin and certain medications like PCSK9 inhibitors and novel RNA-targeted therapies are being investigated for their potential to lower Lp(a) levels.
Awareness and management of other risk factors:
Identifying high Lp(a) levels allows for proactive management of other risk factors, such as blood pressure and diabetes.
Conclusion
Lipoprotein(a) might not be as widely recognized as LDL and HDL cholesterol, but emerging evidence suggests it plays a significant role in cardiovascular health. Understanding the nuances of cholesterol carriers in the blood and the potential risks associated with elevated levels can empower individuals and healthcare professionals to make informed decisions. As research continues to unfold, targeted testing and treatment strategies could contribute to more personalized approaches to reducing cardiovascular risk. Always consult a healthcare provider for personalized guidance on testing and management strategies.