The Mediterranean diet has long been celebrated for its remarkable health benefits and its potential to enhance longevity. Rooted in the traditional eating habits of countries bordering the Mediterranean Sea, this diet emphasizes a rich variety of plant-based foods, healthy fats, and lean proteins. A recent study published in JAMA Network Open offers new insights into how adherence to the Mediterranean diet is associated with reduced all-cause mortality among US women. By examining the underlying biological mechanisms, the study sheds light on the powerful impact this dietary pattern can have on women’s health and longevity. Let’s delve into the findings and understand why the Mediterranean diet continues to be hailed as one of the healthiest dietary patterns.
What is the Mediterranean Diet?
The Mediterranean diet is characterized by a high intake of fruits, vegetables, whole grains, legumes, nuts, and olive oil. It includes moderate consumption of fish and poultry, low consumption of dairy products and red meat, and an emphasis on plant-based foods. Wine is consumed in moderation, typically with meals. This diet is rich in monounsaturated fats, particularly from olive oil, and includes a balance of omega-3 and omega-6 fatty acids.
The Mediterranean diet is inspired by the traditional dietary patterns of countries bordering the Mediterranean Sea, such as Greece, Italy, and Spain. It emphasizes plant-based foods, healthy fats, and lean protein sources, and is associated with numerous health benefits, including reduced risk of chronic diseases and improved longevity.
The Mediterranean diet emphasizes eating:
- Fruits and Vegetables: High intake of a variety of fresh produce.
- Whole Grains: Foods like barley, oats, and brown rice.
- Legumes and Nuts: Beans, lentils, and nuts for protein and fiber.
- Olive Oil: The main source of fat, replacing butter and other fats.
- Fish and Seafood: Regular consumption, particularly of fatty fish like salmon.
- Poultry and Eggs: Moderate amounts for lean protein.
- Dairy: Limited intake, mainly cheese and yogurt.
- Red Meat: Minimal consumption.
- Wine: Keeping alcohol consumption in moderation, typically with meals.
- Herbs and Spices: Used instead of salt for flavoring.
Principles of the Mediterranean Diet
- Variety and Balance: Eat a wide range of foods for a diverse nutrient intake.
- Plant-Based Focus: Make fruits, vegetables, legumes, and nuts the foundation of your diet.
- Healthy Fats: Use olive oil, including nuts and fish, avoiding unhealthy fats.
- Lean Proteins: Opt for fish, poultry, and legumes over red meat.
- Whole Foods: Choose minimally processed foods to retain nutrients.
- Moderation: Practice portion control and moderate alcohol intake.
- Social Eating: Enjoy meals with family and friends to enhance the experience.
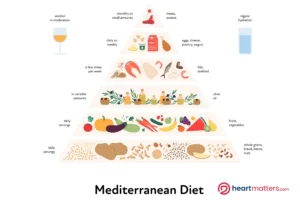
This pyramid visually summarizes the Mediterranean diet’s principles, emphasizing a foundation of physical activity and social interaction, a high intake of plant-based foods, moderate consumption of protein sources and dairy, and a limited intake of red meat and sweets.
Study Overview
The study followed 25,315 healthy women from the Women’s Health Study over an average of 24.7 years. It aimed to see how closely following the Mediterranean diet affected their risk of death from any cause.
Key Findings
The study found that women who followed the Mediterranean diet closely had a lower risk of dying from any cause:
- 8% Lower Risk: For those with moderate adherence.
- 23% Lower Risk: For those with high adherence.
Higher Mediterranean diet adherence was also linked to reduced risks of cardiovascular disease (CVD) and cancer mortality. Compared to those with low adherence scores, women with high adherence scores showed a 17% reduction in CVD mortality and a 20% reduction in cancer mortality.
Scoring Adherence
The Mediterranean diet adherence score ranges from 0 to 9, based on the consumption of nine components:
- Vegetables (excluding potatoes): 1 point if intake is above median.
- Fruits: 1 point if intake is above median.
- Nuts: 1 point if intake is above median.
- Whole Grains: 1 point if intake is above median.
- Legumes: 1 point if intake is above median.
- Fish: 1 point if intake is above median.
- Monounsaturated to Saturated Fat Ratio: 1 point if above median.
- Red and Processed Meats: 1 point if intake is below median.
- Alcohol: 1 point if intake is between 5 and 15 grams per day (equivalent to one drink).
Biological Mechanisms
To unravel the biological mechanisms underlying the reduced mortality risk, the study examined 33 blood biomarkers related to lipid, lipoprotein, apolipoprotein, inflammation, insulin resistance, and metabolism measurements. The analysis revealed that small molecule metabolites and inflammatory biomarkers contributed the most to the lower mortality risk, explaining 14.8% and 13.0% of the association, respectively. Triglyceride-rich lipoproteins, body mass index, and insulin resistance played significant roles, explaining 10.2%, 10.2%, and 7.4% of the association, respectively.
Interestingly, standard cholesterol or glycemic measures had minimal contributions to the lower mortality risk associated with adherence to the Mediterranean diet. This suggests that the Mediterranean diet’s benefits extend beyond traditional markers of cardiovascular health, emphasizing the importance of considering a holistic approach to dietary patterns.
The study also looked at how the diet affects various health markers:
- Inflammation and Metabolism: Reduced inflammation and better metabolic health significantly contributed to the lower risk of death.
- Insulin Sensitivity and Weight Management: Better blood sugar control and weight maintenance.

Practical Tips for Adopting the Mediterranean Diet
- Focus on Plant-Based Foods: Fill your plate with vegetables, fruits, legumes, and whole grains.
- Choose Healthy Fats: Use olive oil and include nuts and seeds.
- Opt for Fish and Poultry: Prefer these over red meat.
- Avoid Processed Foods: Stick to whole, unprocessed foods.
- Enjoy Meals Socially: Eat with family and friends.
- Moderate Alcohol: If you drink, do so in moderation, preferably wine with meals.
Conclusion
The Mediterranean diet offers a holistic approach to health and well-being, emphasizing balanced nutrition and a sustainable lifestyle. The Women’s Health Study findings underscore the diet’s potential to reduce mortality and improve overall health for women. By embracing the Mediterranean diet, women can savor various delicious foods while significantly enhancing their longevity and quality of life. This evidence-based dietary pattern supports long-term health and promotes a vibrant and fulfilling lifestyle, making it an invaluable choice for those seeking to optimize their well-being.










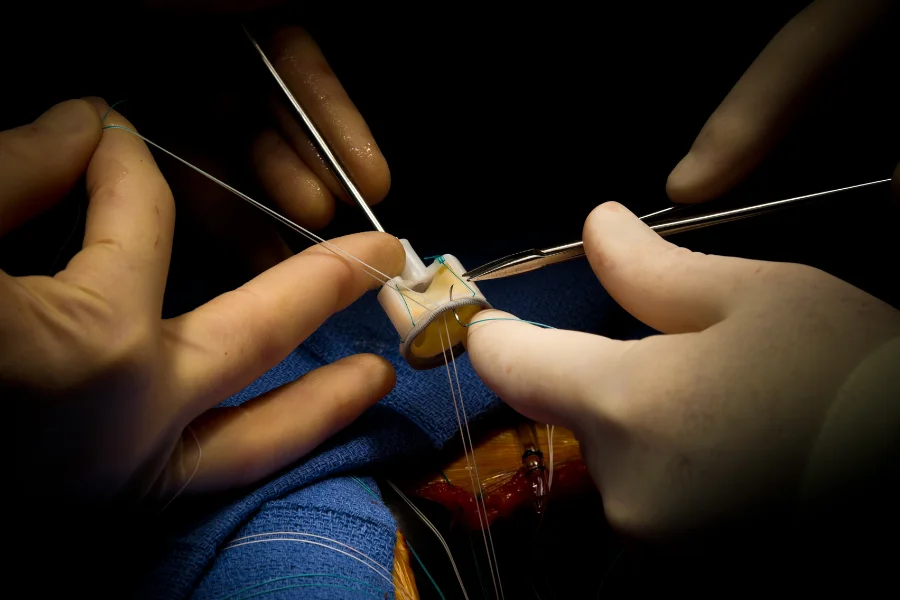
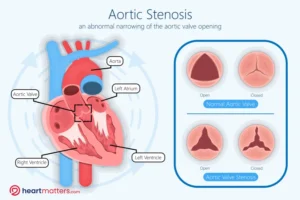
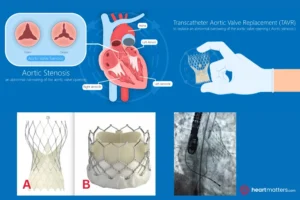
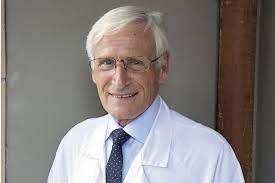 Prof Alain Cribier’s pioneering spirit and unwavering dedication to advancing cardiovascular care through transcatheter interventions have left an indelible mark on the field. As the visionary who first performed aortic balloon valvuloplasty and pioneered Transcatheter Aortic Valve Replacement (TAVR), Prof Cribier’s legacy will continue to inspire generations of clinicians and researchers as we strive to push the boundaries of possibility and improve patient outcomes. Among his career highlights, Cribier performed the first balloon aortic valvuloplasty in 1985 but soon realized its initial success would not last because of restenosis. In the 1990s, he began exploring the possibility of using a balloon-expandable valve stent to prevent restenosis and replace the diseased aortic valve. On April 16, 2002, this vision finally became a reality when Cribier and his colleagues performed the first TAVR. Since then, thousands of patients previously considered inoperable have benefitted from TAVR.
Prof Alain Cribier’s pioneering spirit and unwavering dedication to advancing cardiovascular care through transcatheter interventions have left an indelible mark on the field. As the visionary who first performed aortic balloon valvuloplasty and pioneered Transcatheter Aortic Valve Replacement (TAVR), Prof Cribier’s legacy will continue to inspire generations of clinicians and researchers as we strive to push the boundaries of possibility and improve patient outcomes. Among his career highlights, Cribier performed the first balloon aortic valvuloplasty in 1985 but soon realized its initial success would not last because of restenosis. In the 1990s, he began exploring the possibility of using a balloon-expandable valve stent to prevent restenosis and replace the diseased aortic valve. On April 16, 2002, this vision finally became a reality when Cribier and his colleagues performed the first TAVR. Since then, thousands of patients previously considered inoperable have benefitted from TAVR.