Inflammation is a natural response of the body’s immune system to fight off infections and injuries. However, chronic inflammation can contribute to the development and progression of cardiovascular disease. This article will discuss the importance of inflammation in cardiovascular disease and how to reduce inflammation to improve cardiovascular health.
Inflammation and Cardiovascular Disease
Inflammation is the body’s natural response to injury or infection. It’s a complex biological process that involves the activation of the immune system to protect tissues and initiate the healing process. While inflammation is a critical defense mechanism, chronic or persistent inflammation can harm overall health, particularly cardiovascular wellness.
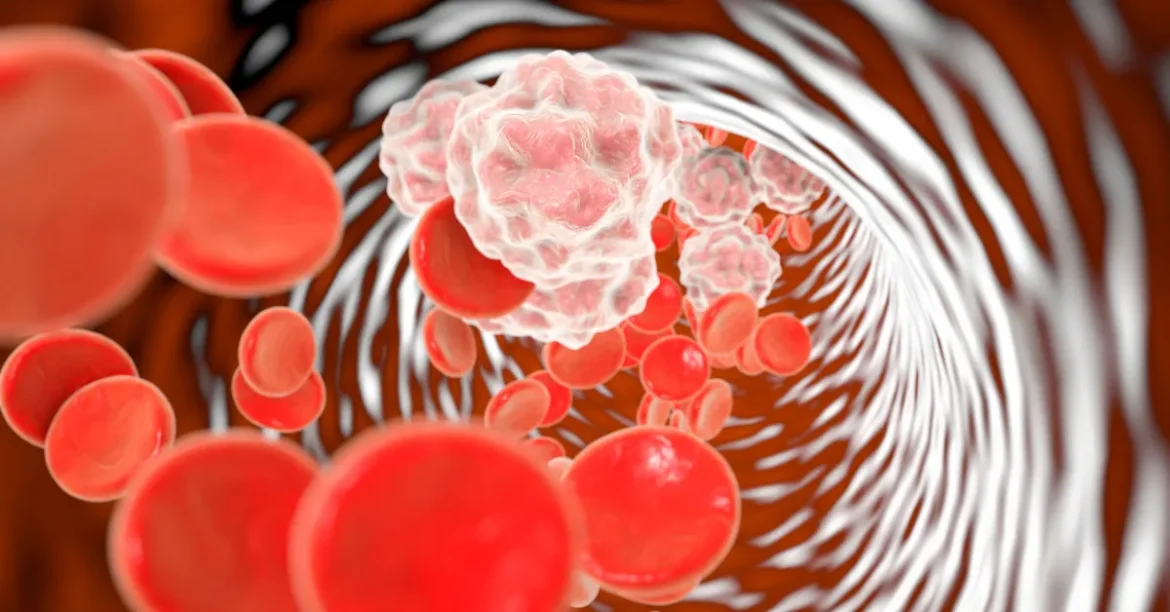
At its core, inflammation is a defense mechanism triggered by the body’s immune system. When tissues are damaged by injury, infection, or toxins, the immune system releases substances, including white blood cells and inflammatory mediators, to combat the threat and repair the damage. This acute inflammatory response is essential for initiating the healing process and restoring tissue function.
However, when inflammation becomes chronic, it can contribute to the development and progression of various diseases, including cardiovascular conditions. Chronic inflammation can damage blood vessels, promote the formation of arterial plaques, and contribute to the narrowing of arteries, increasing the risk of heart disease, stroke, and other cardiovascular complications.
In recent years, researchers have increasingly recognized the role of inflammation in cardiovascular health. Studies have shown that chronic low-grade inflammation is associated with atherosclerosis, a condition characterized by the buildup of plaque in the arteries, as well as other cardiovascular risk factors such as hypertension, obesity, and diabetes.
Reducing Inflammation to Improve Cardiovascular Health
Reducing inflammation is a vital strategy for enhancing cardiovascular health. Numerous conventional risk factors associated with cardiovascular diseases can directly or indirectly activate inflammatory cells, exacerbating inflammation. These inflammatory cells play an active role within arterial plaques, potentially destabilizing them and increasing the risk of complications such as heart attacks or strokes.
Here are some tips to help reduce inflammation:
- Follow a healthy diet: A diet rich in fruits, vegetables, whole grains, and lean protein can help reduce inflammation. Avoid processed foods, saturated and trans fats, and added sugars.
- Exercise regularly: Regular physical activity can help reduce inflammation and improve cardiovascular health. Aim for at least moderate-intensity exercise most days of the week. This can gradually start with a 10-15 min brisk walk and then slowly build this up to 25-30 min.
- Manage stress: Chronic stress can contribute to inflammation. Practicing relaxation techniques, such as meditation, deep breathing, and yoga, can help reduce stress and inflammation.
- Quit smoking: Smoking is a significant cause of inflammation and can increase the risk of cardiovascular disease. Quitting smoking is one of the best things you can do to reduce inflammation and improve cardiovascular health.
- Maintain a healthy weight: Being overweight or obese can contribute to chronic inflammation. Losing weight and maintaining a healthy weight can help reduce inflammation and improve cardiovascular health.
- Optimizing diabetic control – blood sugar fluctuations together with swings of insulin activity can impact inflammation, and therefore by leveling blood sugars and minimizing spikes can go a long way to establishing diabetes, improving cardiovascular health, and controlling inflammation
In conclusion, inflammation is an important contributor to cardiovascular disease but one that is not generally appreciated. Reducing inflammation can be an important strategy for improving cardiovascular health. Follow a healthy diet, exercise regularly, manage stress, quit smoking, and maintain a healthy weight to reduce inflammation and improve cardiovascular health. With a comprehensive approach that addresses traditional risk factors and underlying inflammation, we can take significant strides toward promoting heart health and preventing cardiovascular disease in our communities.
Heart Matters, edited by cardiologist Professor Peter Barlis, is a trusted resource that offers clear and accurate information on cardiovascular health. It bridges the gap between scientific research and everyday understanding, empowering you to make informed choices and take an active role in supporting your heart health.