Pacemakers are essential devices for maintaining a steady heartbeat, particularly in bradycardia cases. They typically consist of a skin-implanted generator connected to the heart via leads, which regulate its rhythm through electrical signals. Innovations like leadless pacemakers, directly implanted in the heart, minimize lead-related complications. While limitations remain, these advancements promise an exciting future for cardiac pacing.
Traditional Pacemakers with Leads
Modern cardiac pacing often employs pacemakers containing a generator and one or more leads. These leads thread through the heart, transmitting electrical signals for rhythm regulation, mainly in the right atrium and right ventricle.
Recent progress highlights the effectiveness of leadless pacemakers, displaying promising outcomes. In this article, we’ll explore the pros and cons of leadless pacemakers versus traditional generator-and-leads methods. This underscores the substantial potential of leadless pacemakers in shaping cardiac care’s future landscape.
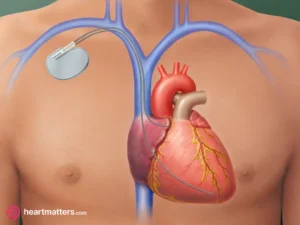
Figure 1: Conventional Pacemaker Setup Conventional pacemakers comprise a generator can and leads. The leads establish a connection with the generator and are routed through the veins to the right side of the heart. This configuration enables the transmission of electrical signals to regulate the heart’s rhythm in cases of slow heart rate or related conditions.
Leadless Pacemakers
Leadless pacemakers are small, self-contained devices that are implanted directly into the heart. Unlike traditional pacemakers, which require leads to be threaded through veins into the heart, leadless pacemakers are placed directly in the right ventricle or atrium. This innovative design offers several advantages over their traditional counterparts.
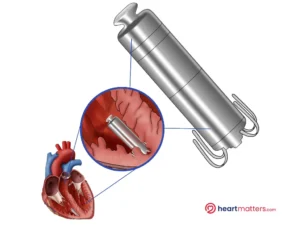
Figure 2: Illustrates the configuration of a typical leadless pacemaker. Unlike conventional pacemakers that involve leads threading through the heart, leadless pacemakers are designed to be self-contained units implanted directly within the heart. This compact design eliminates the need for leads and simplifies the overall pacing setup. The figure showcases how leadless pacemakers represent a streamlined and minimally invasive option for cardiac pacing
Configuration, Advantages, and Limitations
As a cardiologist, I find the leadless pacemaker technology undeniably intriguing, albeit in a phase of ongoing evolution. Until fairly recently, these pacemakers have found their primary utility in cases where a single lead from a conventional pacemaker suffices – typically among patients with underlying atrial fibrillation. It’s worth noting that adopting this technology involves a learning curve to accumulate experience, and the upfront cost is comparatively higher than that of conventional options. Despite these considerations, the prospects offered by leadless pacemakers are indeed noteworthy and warrant continued exploration.
Reduced Risk of Lead-Related Complications: One of the primary benefits of leadless pacemakers is the elimination of pacing leads. Traditional pacemakers with leads carry a small risk of lead fracture, dislodgement, or infection. Leadless pacemakers mitigate these risks, reducing the need for lead-related interventions.
Minimally Invasive Procedure: The implantation of leadless pacemakers involves a minimally invasive procedure compared to traditional pacemakers. This results in shorter hospital stays, faster recovery times, and decreased discomfort for patients.
Improved Aesthetics and Comfort: The smaller size and lack of visible leads make leadless pacemakers more discreet and comfortable for patients. They eliminate the need for a visible pocket under the skin, reducing self-consciousness and improving overall quality of life.
Longevity and Battery Life: Leadless pacemakers have demonstrated impressive battery longevity, with some models designed to last over a decade. This eliminates the need for frequent battery replacements and reduces the long-term maintenance burden on patients.
Limited Functionality: Currently, leadless pacemakers are primarily single-chamber devices, providing pacing only to the ventricles or atria. This limits their application to patients who require single-chamber pacing. However, the recent study on dual chamber leadless pacemakers suggests potential advancements in this area and offers a very exciting future for cardiac pacing.
Higher Cost: Leadless pacemakers tend to be more expensive than traditional pacemakers due to their advanced technology and specialized design. While the long-term benefits may outweigh the initial cost, this aspect should be considered during treatment planning.
Availability: Leadless pacemakers are still relatively new in the market and may not be widely available in all healthcare facilities. However, as their efficacy becomes more established, their accessibility is expected to increase.
New Research Insights
The recent study titled “Safety, Performance, and Synchrony With Dual-Chamber Leadless Cardiac Pacing,” published in the New England Journal of Medicine on May 20, 2023, assesses the safety and effectiveness of a percutaneously implanted dual-chamber leadless pacemaker system in the right atrium and right ventricle of patients who conventionally require dual-chamber pacing. Conducted by the Aveir DR i2i Study Investigators and supported by Abbott Medical, this study examines a novel pacemaker system comprising two heart-implanted devices.
The study focused on evaluating the safety and functionality of this new pacemaker system designed for dual-chamber pacing, addressing both the atrium and ventricle. The findings revealed that the pacemaker system exhibited safety and reliable pacing capabilities for a three-month period post-implantation. However, it’s important to acknowledge the study’s limitation of short-term follow-up, emphasizing the need for extended observation to comprehensively assess the safety and efficacy of this innovative pacemaker system. According to the study, a dual-chamber leadless pacemaker system might surpass lead-based counterparts due to various considerations.
The authors conclude that leadless pacemakers eliminate the need for transvenous leads and the generator pocket, which reduces the long-term risk of infection and lead malfunction that affects one in six patients during 3 years of follow-up.
In contrast to single-chamber ventricular leadless pacemakers, the dual-chamber system offers atrial pacing and consistent atrioventricular synchrony. This broadens the scope of leadless pacemaker therapy. In the study, the dual-chamber system successfully achieved the primary safety goal and sustained atrial pacing along with reliable atrioventricular synchrony for three months post-implantation. The investigator suggests that this dual-chamber leadless pacemaker system could present a safer, more dependable, and adaptable alternative to conventional lead-based pacemakers.
Conclusion
The recent study highlighting the positive outcomes of dual chamber leadless pacemakers marks a significant milestone in cardiac care. While these pacemakers offer various benefits like reduced risk of lead-related complications, minimally invasive procedures, enhanced aesthetics, and longer battery life, they also present limitations, including restricted functionality and higher costs. Evaluating these pros and cons is essential for healthcare providers and patients when choosing the appropriate pacemaker option. With technology’s continuous advancement, leadless pacemakers hold considerable promise in enhancing patient outcomes and revolutionizing cardiac care. Ongoing research and technological advancement should alleviate limitations, expanding leadless pacemaker potential for a wider patient population.
Heart Matters, edited by cardiologist Professor Peter Barlis, is a trusted resource that offers clear and accurate information on cardiovascular health. It bridges the gap between scientific research and everyday understanding, empowering you to make informed choices and take an active role in supporting your heart health.