Electrocardiograms, commonly known as ECGs, play an essential role in cardiology. These diagnostic tools are simple to perform and offer insights into the heart’s electrical activity, aiding in assessing heart health. This guide will explore ECGs’ significance, interpretation, and role in cardiovascular care.
What is an ECG?
An Electrocardiogram, commonly referred to as an ECG or EKG (the ‘K’ denoting the German spelling “Elektrokardiogramm”), is a widely used non-invasive diagnostic test employed in the field of cardiology. It involves the placement of small, adhesive electrodes on specific areas of the skin, typically on the chest, arms, and legs. These electrodes serve as conduits, connecting to a specialized machine known as an ECG recorder.
The core function of the ECG procedure is to capture and record the heart’s electrical signals in real time. This process allows a visual representation, often depicted as a series of waveforms, which graphically illustrates the heart’s electrical activity.

An ECG is a commonly performed test where electrodes are positioned on the chest, arms, and legs, offering different perspectives of the heart. During this painless and quick procedure, the individual remains still for a few seconds as the machine records the heart’s electrical tracings, all of which combine to provide a snapshot of the heart’s beat, rhythm, and overall health.
The significance of an ECG lies in its ability to serve as a diagnostic tool, aiding healthcare professionals in various critical aspects of cardiac care. Firstly, it plays a vital role in identifying irregularities or abnormalities in the heart’s rhythm, highlighting potential issues such as arrhythmias. Additionally, an ECG can assist in detecting damage to the heart muscle, often indicative of conditions like myocardial infarctions or heart attacks. Moreover, it is a valuable tool for monitoring the effectiveness of ongoing treatments and interventions for cardiac conditions.
The ECG is a fundamental diagnostic test routinely administered by paramedics and in the emergency department, playing a critical role in swiftly ruling out an acute heart attack. Its primary focus here is on identifying a specific change: the elevation of the ST segment on the ECG, a critical indicator of an acute blockage and heart attack.
Types of ECG: Resting ECG and Stress ECG
Electrocardiograms (ECGs) come in various forms tailored to specific diagnostic needs. Two common types are the resting ECG and the stress ECG, each serving a unique purpose in cardiac assessment.
Resting ECG:
The resting ECG, often called a standard ECG, is one of the most commonly performed cardiac tests. During this test, the patient lies still, and electrodes are placed on the chest, arms, and legs to record the heart’s electrical activity at rest. Resting ECGs provide a snapshot of the heart’s electrical activity in a relaxed state, offering valuable insights into overall cardiac health.
Stress ECG (Exercise ECG or Treadmill Test):
The stress ECG, or the exercise ECG or treadmill test, involves recording the heart’s electrical activity. At the same time, the patient undergoes controlled physical stress, usually through exercise on a treadmill or stationary bicycle. This type of ECG is primarily used to:
- Assess the heart’s response to increased workload and exercise.
- Detect exercise-induced irregularities in heart rhythm.
- Identify reduced blood flow to the heart muscles, indicative of coronary artery disease.
- Evaluate symptoms such as chest pain, shortness of breath, or palpitations that may occur during physical exertion.
Stress ECGs provide dynamic data, showcasing how the heart functions under stress, which can be invaluable in diagnosing certain heart conditions.
How is an ECG performed?
An ECG is a painless and non-invasive test that typically takes just a few minutes to complete. Here’s what you can expect during an ECG:
- Preparation: You will be asked to remove your shirt and lie on a table. The technician will clean several areas of your body and attach small electrodes to each one.
- Recording: The technician will start the ECG recording by turning on the machine. You will be asked to lie still and breathe normally during the test.
- Interpretation: A healthcare professional will interpret the results after the ECG.
How can an electrocardiogram help?
An ECG is a valuable tool that offers healthcare professionals crucial insights into the heart’s function and overall health. It is employed in conjunction with a comprehensive clinical assessment and potentially with other diagnostic tests, such as echocardiograms (heart ultrasounds) or holter monitors, and can aid in:
- Evaluation of Symptoms: One of the primary indications for an ECG is to assess individuals presenting with symptoms such as chest pain, shortness of breath, or palpitations. The ECG provides crucial insights into the heart’s electrical activity, aiding in the rapid identification of potential cardiac issues and guiding immediate medical interventions.
- Risk Assessment: In patients with risk factors for heart disease, such as high blood pressure, diabetes, or a family history of heart disease, an ECG can be instrumental in evaluating their risk profile. Regular ECG monitoring can assist healthcare providers in identifying early signs of heart problems, allowing for timely intervention and lifestyle adjustments.
- Treatment Monitoring: ECGs are routinely utilized to monitor how the heart responds to medications or other therapeutic interventions. This monitoring is crucial for healthcare professionals to assess treatment effectiveness and make necessary adjustments to optimize patient outcomes. For example, certain medications can impact the heart’s electrical conduction, potentially prolonging the QT interval and increasing vulnerability to problems.
- Rhythm Assessment: The ECG excels in detecting heart rhythm abnormalities, such as atrial fibrillation (AF). By identifying irregular heart rhythms, healthcare providers can effectively tailor treatment strategies to manage and mitigate the associated risks.
The ECG is a versatile and indispensable tool in cardiology, addressing a wide spectrum of diagnostic needs. Its swift provision of crucial heart health information has become a cornerstone in cardiovascular medicine, aiding early diagnosis, informed treatment, and better patient care.
What do the results of an ECG mean?
The results of an ECG can provide insights into:
Heart rhythm: The ECG can detect whether the heart rhythm is regular or irregular. An irregular rhythm may indicate atrial fibrillation, while a slow or fast rhythm may indicate bradycardia or tachycardia.
Heart rate: The ECG can measure the heart rate and assess whether it is too fast or slow.
Heart damage: The ECG can show whether there is damage to the heart muscle, such as from a heart attack or other cardiac event.
Other abnormalities: The ECG can detect other abnormalities in the heart’s electrical activity, such as conduction delays or abnormalities in the intervals between heartbeats.
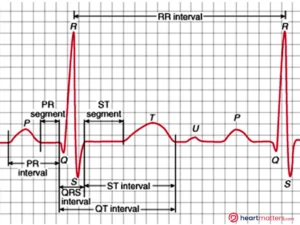
The ECG tracing provides a detailed look at the heart’s electrical activity. The P-wave indicates when the upper chambers of the heart contract, the QRS complex represents the lower chambers contracting, the ST segment offers insights into the early phase of the lower chambers relaxing, and the T-wave signifies the complete heart relaxation. These patterns help healthcare professionals assess heart function and guide treatment strategies.
Conclusion
In conclusion, the electrocardiogram (ECG) stands as a fundamental and accessible diagnostic tool in the realm of cardiovascular medicine. Its simplicity and non-invasive nature make it an invaluable asset in heart health evaluation. Often providing a snapshot of the heart’s electrical activity, an ECG can complement other diagnostic tests and aid healthcare professionals in diagnosing a wide range of heart conditions. Whether you are presenting with symptoms or have risk factors for heart disease, the ECG is a valuable component in the comprehensive assessment of your cardiovascular health.