When it comes to visualising the heart, echocardiography is a powerful and widely used imaging technique. For most people, a standard echocardiogram taken through the chest wall — called a transthoracic echocardiogram (TTE) — provides enough information. However, when greater detail is needed, doctors may recommend a transesophageal echocardiogram, or TEE, to gain a clearer and closer view of the heart’s internal structures.
TEE involves placing a small ultrasound probe into the oesophagus — the tube that connects your mouth to your stomach. Because the oesophagus lies directly behind the heart, this positioning allows the probe to capture high-quality, unobstructed images of the heart and surrounding vessels.
In this article, we’ll explore what TEE is, when it is used, and what to expect during the procedure.
What Is a Transesophageal Echocardiogram?
A transesophageal echocardiogram is a specialised form of heart ultrasound. Instead of using a probe on the chest, the ultrasound probe is gently passed into the oesophagus. This brings it very close to the heart, allowing for exceptionally detailed images without interference from the chest wall, lungs, or ribs.
TEE is particularly valuable when standard echocardiography does not provide enough clarity or when precise imaging is essential for diagnosis or treatment planning.
When is TEE Used?
TEE is used in a variety of clinical situations where precise imaging is essential for diagnosis or treatment planning. Some of the most common indications for TEE include:
Heart Valve Evaluation: TEE is often used to assess the function and structure of heart valves. This is particularly valuable before surgeries to repair or replace heart valves.
Detecting Heart Defects: TEE is effective in detecting septal defects, such as an atrial septal defect (ASD) or a patent foramen ovale (PFO). These conditions involve a hole in the heart’s septum (the wall separating the atria) and can lead to complications if left untreated.
Endocarditis Diagnosis: In cases of endocarditis, an infection of the inner lining and valves of the heart, TEE can detect abnormal growths on the heart valves called vegetations, which are key indicators of this infection.
Identifying Blood Clots and Aortic Disease: TEE is particularly useful for detecting blood clots, especially in the left atrium and its appendage, a site where clots can sometimes form and increase the risk of stroke. It’s also used to evaluate aortic dissection or aneurysm.
Guiding Cardiac Surgery: TEE may be used in the operating room to help guide surgeons during complex cardiac procedures, providing real-time imaging that ensures accuracy.
What to Expect During the TEE Procedure
For patients who are scheduled for a TEE, understanding the steps involved can help ease any anxiety. Here’s a breakdown of what the procedure generally involves:
Preparation:
You’ll typically need to fast for at least 6 hours before the procedure.
A mild sedative will be administered to help you relax, and your throat may be numbed with a local anesthetic spray to reduce discomfort during the procedure.
Insertion of the Probe:
The TEE probe is a flexible tube with a small ultrasound transducer at the tip. Your healthcare provider will gently guide this probe through your mouth and into your esophagus. Since the esophagus is located just behind the heart, this allows the probe to capture close, clear images.
Imaging the Heart:
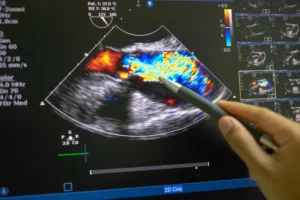
The probe sends out sound waves that bounce off your heart and are converted into real-time images on a monitor. This provides detailed visual information about the heart’s structure, blood flow, and any abnormalities present.
Monitoring and Duration:
The entire TEE procedure typically lasts between 30 and 60 minutes. Throughout the procedure, medical staff will monitor your heart rate, blood pressure, and oxygen levels to ensure safety.
Post-Procedure Care:
After the procedure, you may experience a mild sore throat for a few hours.
Avoid eating or drinking anything until the numbness in your throat wears off, to prevent choking.
Due to the effects of sedation, you may need someone to drive you home afterward.
Benefits of TEE
TEE provides several advantages over standard echocardiography:
High-Resolution Imaging: By capturing images from within the esophagus, TEE offers unparalleled clarity, which is especially useful for identifying structural heart problems.
Accuracy: TEE is known for its accuracy in diagnosing conditions related to heart valves, clots, and complex heart defects.
Minimally Invasive Option: Compared to other techniques requiring more invasive measures, TEE is a minimally invasive procedure with a low risk of complications.
Risks and Considerations
Although TEE is generally safe, there are some low but notable risks:
Discomfort or Throat Irritation: Patients may experience some throat soreness afterward.
Esophageal Injury: While rare, there is a slight risk of injury to the esophagus during probe insertion.
Sedation Reactions: Sedation reactions are uncommon but possible. Patients are closely monitored to reduce any potential risks.
Additionally, individuals with esophageal conditions, such as strictures or severe swallowing disorders, may not be ideal candidates for TEE.
Conclusion
Transesophageal echocardiography is a valuable tool for obtaining detailed information about heart structure and function. Although most relevant information can be obtained from a standard non-invasive transthoracic echo scan, teh TEE is especially helpful for diagnosing heart valve issues, blood clots, infections, and structural abnormalities. By providing high-resolution images, TEE plays a crucial role in helping cardiologists and surgeons plan precise treatments.










