Discussing medication with patients is integral to better health outcomes. In this article, we’ll elaborate on a commonly used class of medicine found worldwide – Angiotensin 2 Receptor Blockers (ARBs) – and their significant impact on maintaining and improving heart health. Let’s explore how ARBs work, their benefits, and why they are often recommended for patients with various cardiovascular conditions.
Exploring the Mechanism of ARB Medicines
To begin, let’s delve into the fundamental mechanisms of ARB medications and their role in our physiology. Angiotensin Receptor Blockers (ARBs) represent a class of pharmaceuticals primarily employed in managing hypertension (high blood pressure) and various heart-related conditions. The essence of how ARBs function lies in their ability to counteract the actions of a hormone known as angiotensin II.
Angiotensin II is a potent vasoconstrictor that narrows blood vessels, leading to an elevation in blood pressure. This hormone’s influence can be detrimental to cardiovascular health. However, ARBs step in as mediators of change. These medications effectively block the effects of angiotensin II, a pivotal action that holds the key to their therapeutic effect. By inhibiting the vasoconstrictive effects of angiotensin II, ARBs promote the relaxation and dilation of blood vessels. This, in turn, results in a notable reduction in blood pressure levels, contributing to better heart health.
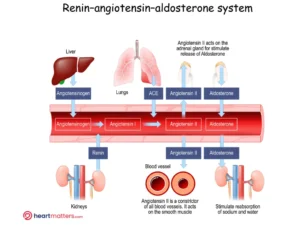
This figure illustrates the Renin-Angiotensin-Aldosterone System (RAAS) and the role of Angiotensin 2 Receptor Blockers (ARBs). In response to low blood pressure, the kidneys release renin, producing angiotensin II—a potent vasoconstrictor (narrowing of blood vessels) that increases blood pressure. ARBs block angiotensin II’s action, causing blood vessels to relax and blood pressure to decrease. ARBs are essential in managing hypertension and promoting heart health.
Benefits of ARB Medicines for Heart Health
- Managing Hypertension: ARBs are considered one of the most effective treatments for hypertension, a leading risk factor for heart disease and stroke. By lowering blood pressure, ARBs decrease the strain on the heart and blood vessels, reducing the risk of cardiovascular complications.
- Protecting the Heart: Beyond their ability to lower blood pressure, ARB medications demonstrate direct advantages for the heart. They play a pivotal role in averting and reversing the adverse changes that frequently transpire in heart conditions like heart failure or post-heart attack. ARBs achieve this by obstructing the effects of angiotensin II, which subsequently diminishes inflammation and oxidative stress. This protective action preserves heart function and enhances overall cardiac well-being. It’s important to note that even in patients with normal blood pressure, we often prescribe ARBs due to these additional benefits, illustrating their significance beyond blood pressure control.
- Managing Diabetic Nephropathy: Diabetic nephropathy, a kidney disease caused by diabetes, is another condition where ARBs play a crucial role. By dilating the blood vessels within the kidneys and reducing pressure on the filtration system, ARBs help slow the progression of kidney damage, preserving renal function in diabetic patients and reducing protein loss in the kidneys.
- Combating Stroke Risk: High blood pressure is a significant risk factor for stroke, and ARBs have shown promise in reducing this risk. By maintaining optimal blood pressure levels, ARBs contribute to the prevention of both ischemic and hemorrhagic strokes, improving overall cerebrovascular health.
- Cardiovascular Protection in High-Risk Patients: Patients with existing heart conditions, such as coronary artery disease or previous heart attacks, greatly benefit from ARB therapy. These medicines can help reduce the risk of further complications after a heart attack and improve overall cardiovascular outcomes.

Commonly Prescribed ARB Medications
Regarding ARB medications, several options are available, and your healthcare provider will select the most appropriate one based on your unique requirements. Some frequently prescribed ARBs, along with their generic and trade names, include:
- Losartan (Cozaar)
- Valsartan (Diovan)
- Candesartan (Atacand)
- Irbesartan (Avapro, Karvea)
- Telmisartan (Micardis)
- Olmesartan (Benicar, Olmetec)
It’s essential to remember that individual responses to these medications can vary. Your healthcare professional will closely monitor your progress to ensure the ARB effectively addresses your needs.
Combination Therapies
In many cases, healthcare providers employ combination therapies to enhance the effectiveness of ARBs in managing blood pressure and cardiovascular conditions. Combining ARBs with other medication classes like Hydrochlorothiazide (HCT) and Amlodipine has become a well-established approach.
-
Hydrochlorothiazide (HCT): HCT is a diuretic medication commonly used to treat high blood pressure (hypertension) and reduce fluid retention in conditions like heart failure. It works by increasing the elimination of excess salt and water from the body through urine. This reduction in fluid volume helps lower blood pressure, making it an effective partner in combination therapies with ARBs.
-
Amlodipine: Amlodipine is a calcium channel blocker used to treat high blood pressure and chest pain (angina). It works by relaxing the blood vessels, allowing for smoother blood flow and reducing the workload on the heart. When combined with ARBs, amlodipine can help further lower blood pressure and improve cardiovascular function.
When used in conjunction with ARBs, these medications create powerful combination therapies that target different aspects of blood pressure regulation and cardiovascular health, offering comprehensive treatment options for patients with various cardiovascular conditions.
Potential Side Effects
While ARB medicines are generally well-tolerated, it’s essential to be aware of potential side effects. It’s crucial to remember that not everyone will experience these side effects, and the benefits of ARBs often outweigh the risks. Always consult with your healthcare provider if you have any concerns or questions.
- Hypotension (Low Blood Pressure): One of the most common side effects of ARBs is a temporary drop in blood pressure. This can cause dizziness, lightheadedness, or fainting, particularly when standing up quickly. It’s important to rise slowly from a seated or lying position to minimize this effect, particularly in the early stages of starting the medication. Contact your healthcare provider if you experience severe or prolonged low blood pressure symptoms.
- Hyperkalemia (High Potassium Levels): ARBs can sometimes lead to increased potassium levels in the blood. This is more likely to occur in individuals with pre-existing kidney problems or those taking other medications that affect potassium levels. Symptoms of hyperkalemia may include muscle weakness, palpitations, or an irregular heartbeat. Regular monitoring of potassium levels by your healthcare provider will help prevent any complications.
- Allergic Reactions: While rare, some individuals may experience allergic reactions to ARB medications. Signs of an allergic reaction include rash, itching, swelling of the face, lips, tongue, or throat, and difficulty breathing. Seek immediate medical attention if you experience these symptoms.
- Renal Impairment: In rare cases, ARBs can affect kidney function, particularly in individuals with pre-existing kidney disease or reduced kidney function. Regular monitoring of kidney function through blood tests is essential during ARB therapy to ensure any potential issues are promptly addressed.
- Other Side Effects: Additional side effects that may occur but are less common include headache, fatigue, diarrhea, nausea, and cough. These symptoms are generally mild and tend to resolve on their own. However, if they persist or become bothersome, inform your healthcare provider.
It’s important to emphasize that the above side effects are not exhaustive, and individual medication responses can vary. Your healthcare provider will closely monitor your progress and make necessary adjustments to ensure the best possible outcomes while minimizing potential risks.
Conclusion
Angiotensin 2 Receptor Blockers (ARBs) emerge as commonly used and well-tolerated medicines with pivotal roles in cardiovascular health. They are primary choices for managing hypertension and heart-related conditions, known for their effectiveness and tolerability. Beyond their blood pressure-lowering abilities, ARBs are crucial in preventing detrimental cardiac remodeling, reducing inflammation, and alleviating oxidative stress, thereby contributing to overall heart health. These medications have become cornerstone treatments for various cardiovascular conditions, offering practical solutions and improved quality of life for many individuals worldwide.
Heart Matters, edited by cardiologist Professor Peter Barlis, is a trusted resource that offers clear and accurate information on cardiovascular health. It bridges the gap between scientific research and everyday understanding, empowering you to make informed choices and take an active role in supporting your heart health.









