In this article, we’ll explore a common yet important health concern that affects many individuals—blood clots. While these formations are crucial for our body’s healing processes, they can also pose risks when they occur unexpectedly or excessively. We’ll delve into the fundamental aspects of blood clots, including their nature, causes, potential complications, and available treatment options. By understanding these essential aspects, you’ll be better equipped to navigate potential blood clot-related issues and proactively approach your well-being.
What are Blood Clots
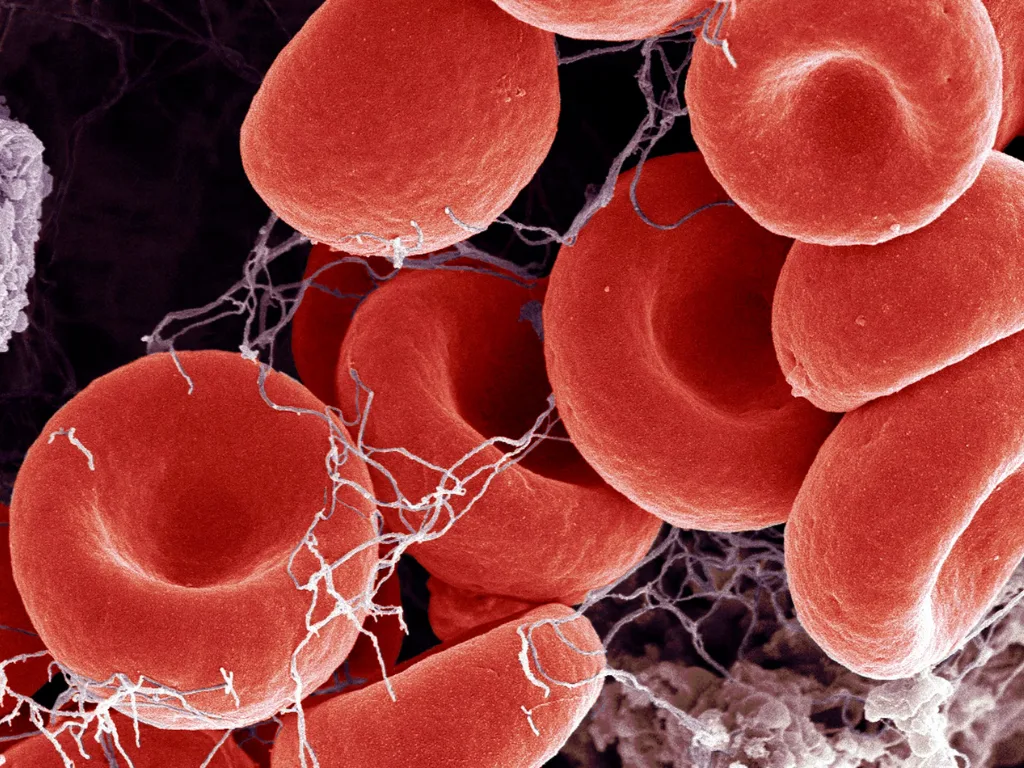
Blood clots, medically referred to as thrombi, are gel-like masses that form when the blood’s components, such as platelets and fibrin, bind together in response to an injury or to prevent excessive bleeding. They play a crucial role in wound healing by stopping bleeding from damaged blood vessels. However, when blood clots form inappropriately or excessively, they can lead to various health complications. Blood clots can be broadly categorized into venous and arterial clots, each with distinct characteristics and potential consequences.
Types of Blood Clots
There are various blood clots, broadly categorized into venous and arterial clots.
Venous Clots:
Venous Thrombosis (Clots): Venous thrombosis, as indicated by its name, occurs within veins and is mainly classified into three types: deep vein thrombosis (DVT), superficial vein thrombosis, and pulmonary embolism (PE). These clots can affect any organ, spanning from the retinal (eye) vein and portal (liver) vein to various other veins. DVT refers explicitly to forming a blood clot within a deep vein, frequently found in the legs or pelvis.
Should a fragment of this clot dislodge and migrate to the lungs, it can result in a pulmonary embolism. The likelihood of experiencing a pulmonary embolism is more significant in deep vein thrombosis (DVT) cases than in superficial thrombosis. Due to this disparity, the treatment approach differs for each condition.
Pulmonary embolism is a serious condition that can cause difficulty breathing, chest pain, and in severe cases, even be life-threatening. Venous clots can impede blood flow and cause swelling, pain, and potentially long-term complications if not managed promptly.
Arterial Clots: Arterial clots develop within arteries, the blood vessels that carry oxygen-rich blood away from the heart to the rest of the body. These clots are commonly associated with conditions like stroke and myocardial infarction, commonly known as a heart attack. Arterial clots can lead to the sudden blockage of blood flow to vital organs. In the case of a stroke, the interruption of blood flow to the brain can result in neurological damage, while a heart attack occurs when the blood supply to the heart muscle is compromised, leading to heart tissue damage. Arterial clots can have severe and often irreversible consequences.
Symptoms of Blood Clots
Depending on their location and severity, blood clots can manifest with various symptoms. Common symptoms include:
-
Swelling: Swelling in the affected area, often in the legs or arms, can indicate a clot obstructing blood flow.
-
Pain or Tenderness: Persistent pain or tenderness in an area on an arm or leg may point to a clot. This may be accompanied by swelling or a change in skin color.
-
Redness or Warmth: Skin that feels warmer to the touch or appears red and inflamed could indicate clot-related inflammation.
-
Shortness of Breath: Sudden difficulty breathing or chest pain might signal a clot in the lungs, known as a pulmonary embolism.
-
Coughing: Coughing, possibly with blood, can indicate a pulmonary embolism.
-
Chest Pain: Severe chest pain, often radiating to the arm, neck, or jaw, might suggest a clot-related heart issue. In cases of PE, chest pain may be worse with inspiration, often called pleuritic chest pain.
-
Numbness or Weakness: Numbness, weakness, or paralysis in the face, arm, or leg could indicate a clot-induced stroke.
-
Headache: A sudden, severe headache might accompany a clot-related stroke.
-
Speech Difficulties: Trouble speaking or understanding speech is another potential sign of a stroke.
-
Change in Vision: Sudden changes in vision, such as blurred vision or loss of vision in one eye, could indicate a clot-related issue.
It’s important to note that these symptoms can vary widely and may not always indicate a blood clot. However, if you experience any of these symptoms or have concerns, seeking prompt medical attention is advisable to determine the cause and receive appropriate care.
Risk Factors for Developing a Blood Clot
Blood clots, essential for wound healing and preventing excessive bleeding, can pose serious health risks when they form inappropriately or excessively. Certain factors and conditions can elevate the likelihood of developing these problematic blood clots. Recognizing these risk factors is crucial for proactive prevention and effective management. Here are some of the key elements and conditions associated with blood clot formation:
-
Deep vein thrombosis (DVT) and Pulmonary Embolism (PE): These occur due to immobility, which can arise from long-haul travel, extended bed rest, or immobilization after surgery.
-
Medical Conditions: Certain medical conditions like cancer and heart arrhythmias e.g., AF, heart failure, and antiphospholipid syndrome, can disrupt normal blood flow and increase clotting risk.
-
Genetics: Genetic factors, such as Factor V Leiden gene or Prothrombin gene mutation, can predispose individuals to blood clot formation.
-
Cardiovascular Health: Conditions like atherosclerosis, which lead to narrowed and hardened arteries, contribute to clot development.
-
Lifestyle Factors: Lifestyle choices like smoking, obesity, and prolonged sitting can elevate the risk of clot formation.
-
Hormones and Medications: Oral contraceptives, hormone therapy drugs, and certain medications can increase clotting risk.
-
COVID-19: Infection with the coronavirus disease 2019 (COVID-19) has been associated with abnormal clotting.
-
Pregnancy: Pregnancy-related changes can impact blood flow and increase the risk of clot development.
-
Family History: A family history of blood clot disorders can indicate a genetic predisposition to clot formation.
Treatment Strategies for Blood Clots
The treatment of blood clots varies depending on their location and your overall health. If you suspect a blood clot and are experiencing symptoms, seeking immediate medical attention is essential.
Progress in research has substantially enhanced both the approaches for preventing and treating blood clots. Current treatments encompass:
1. Anticoagulants: Anticoagulants are medications designed to prevent the formation of blood clots. They work by hindering the clotting process, reducing the risk of clots forming within blood vessels. Anticoagulants are the mainstay of treatment for patients with clots. The other treatment modalities described below apply only to a few patients. For years, Warfarin was the only drug available to treat cloning disorders, however nowadays, we have several newer anticoagulants with excellent efficacy and better safety profiles without the requirement for any regular blood testing.
2. Thrombolytics: Thrombolytics are medications that actively dissolve existing blood clots. They are used to swiftly address clots that have already formed, restoring blood flow and minimizing potential damage, and are only used in an emergency setting.
3. Catheter-Directed Thrombolysis: Catheter-directed thrombolysis involves a specialized procedure. A catheter, a long tube, is carefully inserted and guided toward the location of the blood clot. This catheter delivers clot-dissolving medication directly to the clot, facilitating its dissolution.
4. Thrombectomy: Thrombectomy is a surgical intervention to remove a blood clot physically. This procedure can be particularly effective in restoring normal blood flow, especially in critical situations.
Conclusion
In conclusion, blood clots present a significant medical concern that can have profound implications for individuals’ health and well-being. Understanding the risk factors, symptoms, and preventive measures associated with blood clots is essential in promoting early detection and effective management. As medical research advances, our knowledge of blood clot formation and treatment continues to evolve. By staying informed and adopting healthy lifestyle choices, individuals can take proactive steps to reduce their risk of developing blood clots. Vigilance, regular medical check-ups, and adherence to prescribed treatments can collectively contribute to better outcomes and improved overall health.