Plastics, from food packaging to electronic devices, have become integral to our daily lives. However, the alarming rise in plastic pollution has raised concerns about its impact on human health. A recent New England Journal of Medicine study (linked here) has shed light on a potential link between plastics found in cholesterol deposits inside the carotid artery and future cardiovascular events.
Study Background
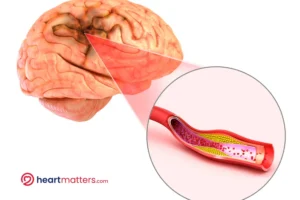
Carotid plaques are deposits of cholesterol, fat, calcium, and other substances that build up inside the carotid arteries, the major blood vessels in the neck that supply blood to the brain, face, and neck (see below figure). Over time, these plaques can narrow the carotid arteries, restricting blood flow to the brain. If a piece of plaque breaks off and travels to the brain, it can block a smaller blood vessel, causing a stroke.
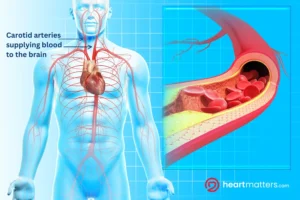
The risk of stroke increases when the carotid arteries become severely narrowed or if a piece of plaque breaks off and causes a blockage in a blood vessel leading to the brain. This can result in a lack of oxygen and nutrients to brain cells, leading to stroke symptoms such as sudden weakness or numbness on one side of the body, difficulty speaking or understanding speech, vision problems, and severe headaches.
Carotid endarterectomy
This is a surgical procedure performed to remove plaque buildup from the carotid arteries. It is typically considered for individuals with significant narrowing (stenosis) of the carotid arteries, usually due to atherosclerosis (plaque buildup).
Carotid endarterectomy is considered when:
Symptoms are present: If an individual experiences symptoms of reduced blood flow to the brain, such as transient ischemic attacks (TIAs) or minor strokes, and diagnostic tests reveal significant narrowing of the carotid arteries, carotid endarterectomy may be recommended to reduce the risk of future strokes.
High-grade stenosis: If imaging tests, such as ultrasound or angiography, show that the carotid artery is severely narrowed (usually greater than 70%) and the individual has not experienced symptoms, carotid endarterectomy may still be considered to prevent future strokes. The decision is always personalized and will occur following discussions with yourself, a neurologist, and the vascular surgeon.
Other factors: The decision to undergo carotid endarterectomy may also consider other factors, such as the individual’s overall health, age, risk factors for stroke (such as smoking, high blood pressure, and diabetes), and plaque in other blood vessels while also considering one’s surgical fitness.
Vascular surgeons typically perform carotid endarterectomy. This procedure involves an incision in the neck to access the carotid artery, removing plaque buildup and repairing the artery.
This illustration depicts a brain with an area of stroke resulting from plaque buildup in the carotid artery. The plaque buildup restricts blood flow to the brain, leading to reduced oxygen supply and tissue damage, characteristic of a stroke. This representation highlights the potential consequences of carotid artery disease, emphasizing the importance of managing plaque buildup to prevent stroke and other related complications.
What This Study Tells Us
The study published on March 7, 2024, in the New England Journal of Medicine (linked here) revealed a significant potential connection between plastic particles found within cholesterol plaques of individuals with narrowed carotid arteries. This intriguing study underscores the widespread presence of plastics in our environment, which, once released into nature, tend to degrade into minuscule fragments. In this investigation, these fragments, categorized as microplastics (less than five millimeters) and nanoplastics (less than 1000 nanometers), were closely examined.
This study explored the relationship between these tiny microplastics and nanoplastics (MNPs), found in carotid artery plaque and the likelihood of cardiovascular events. Researchers conducted a thorough investigation involving patients with asymptomatic carotid artery disease who were scheduled for carotid endarterectomy.
They examined the removed plaque samples using various advanced techniques, including electron microscopy, to detect the presence of MNPs and evaluate inflammatory biomarkers in the samples. The main goal was to determine whether the presence of MNPs was associated with an increased risk of heart attack, stroke, or death.
Findings
This study, which included 312 patients who underwent carotid endarterectomy, showed that microplastics and nanoplastics were detectable in the excised plaque of 58% of the patients.
Patients with evidence of MNPs were younger, more likely to be men, less likely to have hypertension, more likely to have diabetes, cardiovascular disease, and dyslipidemia, and more likely to smoke.
The presence of microplastics or nanoplastics in carotid artery plaque was associated with a subsequent risk of nonfatal myocardial infarction, nonfatal stroke, or death from any cause that was 2.1 times that in patients whose plaques did not contain microplastics or nanoplastics.
How do plastics enter our bodies?
Based on the information provided by the study authors, the sources of microplastics and nanoplastics (MNPs) are as follows:
- Plastic production: The production of plastics is constantly increasing, leading to the widespread distribution of plastic particles in the environment. Plastics can enter the environment through various means, such as ocean currents, atmospheric winds, and terrestrial phenomena.
- Degradation of plastics: Once released into nature, plastics are susceptible to degradation, forming microplastics (particles smaller than 5 mm) and nanoplastics (smaller than 1000 nanometers). This degradation can occur due to various factors, including exposure to sunlight, mechanical abrasion, and chemical breakdown.
- Human activities: Microplastics and nanoplastics can enter the body through ingestion, inhalation, and skin exposure. Humans can be exposed to MNPs through various sources, such as contaminated food and water, air pollution, and contact with plastic-containing products.
Transportation of plastics:
- Ingestion: MNPs can enter the human body by ingesting contaminated food and water. Plastics can accumulate in the gastrointestinal tract and interact with tissues and organs.
- Inhalation: MNPs can also enter the body through air pollution inhalation. Plastic particles can be present in fine particulate matter (PM2.5) and transported long distances by wind.
- Skin exposure: MNPs can interact with the skin and potentially penetrate the body through dermal absorption.

Study Implications
The present study provides strong evidence to link these plastics to cardiovascular disease. The study’s findings suggest that patients with detectable MNPs in their carotid artery plaques are at a higher risk of cardiovascular events than those without MNPs. Moreover, the study highlighted that MNPs could trigger toxic effects and increase inflammatory biomarkers in plaque, further escalating the risk of adverse cardiovascular outcomes.
According to an accompanying Editorial by Dr Philip J. Landrigan, M.D:
Although we do not know what other exposures may have contributed to the adverse outcomes among patients in this study, the finding of microplastics and nanoplastics in plaque tissue is itself a breakthrough discovery that raises a series of urgent questions.
Conclusion
In conclusion, this study illuminates the correlation between microplastics and nanoplastics (MNPs) found within carotid artery plaques and the heightened risk of cardiovascular events. The findings underscore the potential negative impacts of plastic pollution on human health, raising the issue that these considerations extend beyond climate and environmental impact to affect human cardiovascular outcomes directly.
Addressing plastic pollution and its repercussions on human health is critical in safeguarding cardiovascular well-being and public health. Further research is crucial to understand better the mechanisms underlying these associations and to develop effective strategies for mitigating the adverse effects of plastic pollution on cardiovascular health.