As a Cardiologist, I frequently hear patients discussing a dry cough – one of the more common symptoms they encounter. Despite undergoing multiple tests to identify potential causes such as asthma, COVID-19, lung disease, or gastric reflux, the cough persists. It might even be more noticeable during nighttime. So, the question arises: Which medication could be responsible for this? Let’s delve deeper!
If you’ve been diagnosed with hypertension (high blood pressure) and are undergoing medication, you might have experienced a dry cough as a potential side effect. In this article, we will illuminate the relationship between a dry cough and blood pressure medications, specifically focusing on ACE inhibitors (Angiotensin-Converting Enzyme inhibitors). Grasping this connection will aid those on these medications in recognizing and effectively managing this frequently encountered side effect through consultations with their healthcare provider.
Gaining Insight into ACE Inhibitors
ACE inhibitors, a commonly prescribed medication class for managing high blood pressure, work by relaxing blood vessels, minimizing fluid retention, and consequently reducing blood pressure levels. They influence a rather intricate hormonal system in our bodies, known as the renin-angiotensin-aldosterone system, essential for maintaining normal homeostasis.
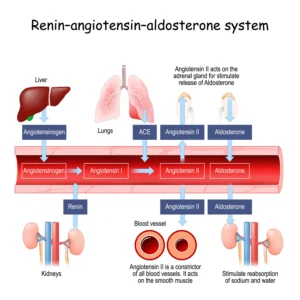
ACE inhibitors function by blocking the ACE receptors, which leads to reduced constriction of blood vessels and the elimination of excess salt and fluids. This mechanism contributes to the reduction of blood pressure.
ACE inhibitors consistently demonstrate cardiovascular protection by improving survival rates and decreasing the risk of significant cardiovascular events. These benefits span diverse patient groups affected by vascular conditions like hypertension, stable coronary artery disease, myocardial infarction (MI), and heart failure (HF). Additionally, ACE inhibitors prove their effectiveness in preventing strokes and delivering cardioprotective and nephroprotective effects for individuals with diabetes.
The cardiovascular advantages of ACE Inhibitors have prompted wide approval from prominent clinical practice guidelines including the European Society of Cardiology (ESC), the American Heart Association (AHA), the American College of Cardiology (ACC), and the Cardiac Society for Australia and New Zealand (CSANZ). Consequently, these guidelines advocate for ACE inhibitors as the preferred choice in managing coronary and atherosclerotic vascular diseases, high blood pressure, heart failure and in the treatment of patients following heart attack (myocardial infarction).
ACE Inhibitors Examples
The Dry Cough Side Effect
The ACE inhibitor cough is often described as persistent and unproductive, meaning it does not produce mucus or phlegm. While the exact mechanism behind this side effect is not fully understood, it is believed to be related to the accumulation of bradykinin, which causes blood vessels to dilate. ACE inhibitors block the breakdown of bradykinin, leading to its increased levels, which can irritate the respiratory tract and trigger a cough reflex.
Taking Control of the Dry Cough
If ACE inhibitors are causing you to experience a dry cough, engaging with your healthcare provider becomes essential. They will evaluate the cough’s severity, assess your condition, and deliberate on potential adjustments or alternatives for your medication routine.
In certain instances, the body may adapt to the medication over time, resolving the cough. Nevertheless, when the cough persists and disrupts your comfort, your healthcare provider might explore transitioning you to a different category of blood pressure medication, such as angiotensin receptor blockers (ARBs). ARBs operate differently from ACE inhibitors and are less likely to induce the dry cough side effect. For milder cases, tweaking the dosage or introducing other blood pressure therapy categories to complement the ACE inhibitor – such as incorporating calcium channel blockers like amlodipine or diuretics like thiazides – could also assist in mitigating the cough.
Angiotensin receptor blockers may be an alternative to ACE inhibitors where cough is persisting.
Conclusion
If you are taking ACE Inhibitors and facing a persistent dry cough, it’s important to recognize that this could be a side effect of the medication. While the ACE inhibitor-induced cough may be bothersome, it should not overshadow the positive impact these medications have on cardiovascular health. By addressing potential side effects in partnership with your healthcare professional, you can strive for optimal heart health while minimizing inconvenience.










