Magnesium has long been a staple in diets globally around the world. Present in abundance in many foods that we regularly consume. From the ages of 14-18, our magnesium requirement starts to increase significantly. Males generally need about 400mg of magnesium a day, and females need approximately 300mg to meet their recommended daily intake, which increases slightly as you age.
The average adult’s dietary intake of magnesium is adequate from milk to various seeds and nuts. However, the Australian Bureau of Statistics demonstrated that about 1 in 3 Australians don’t get enough magnesium and about 50-60% in those over 70 don’t meet their daily magnesium requirement.
So why does magnesium matter?
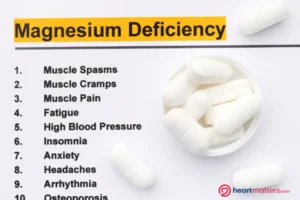
Magnesium has various effects throughout the body, not just on the cardiovascular system, and is thought to enhance sleep quality [1] and muscle recovery post-exercise. [2] But most importantly, studies have demonstrated magnesium deficiency will increase your risk of developing conditions like diabetes or coronary artery disease, as well as increase your risk for stroke. [3]
Through the many effects explained below, this unassuming mineral is a powerhouse that supports cardiovascular and general health and well-being.
Magnesium and heart health
Magnesium and irregular heart rhythms
Magnesium has been shown, through lab-based and real-world clinical research, to positively affect the prevention of irregular heartbeats, such as atrial fibrillation (AF). Several studies have highlighted the potential link between low serum magnesium levels and the development of AF.
In a subgroup analysis of participants in the Framingham-Offspring study (a continuation of the famous long-running FRAMINGHAM study), low-normal blood magnesium was associated with an increased risk of AF in the community, even after adjusting for blood potassium levels [4], when compared to those with higher levels of magnesium within the “normal” range (0.85-1.10). This suggests that Magnesium plays a key role in preventing atrial fibrillation.
Moreover, the role of magnesium in preventing AF after cardiac surgery has been extensively studied. A study in 2023 found that the proportion of patients with postoperative AF was lower in those who received magnesium, suggesting a potential role of magnesium in preventing AF following cardiac surgeries [5].
The link between magnesium and preventing acute bouts of irregular heart rate remains contentious. However, as we’ll learn, the long-term effects of magnesium on your heart make it more than worth it to keep your levels up.
Endothelial Health
Magnesium plays a crucial role in maintaining endothelial function. The endothelium is the microscopic inner lining of all your vessels throughout your body, and a healthy endothelium is central to keeping pathology like plaque and atherosclerosis (causes of coronary artery disease and hypertension) at bay. Endothelial function significantly affects many risk factors for cardiovascular disease, such as hypertension, diabetes or pre-diabetes, and disorders of cholesterol metabolism [6].
Studies have shown that magnesium supplementation in those with stable coronary artery disease can help improve exercise tolerance and blood flow versus placebo. [7]
Heart Remodelling
In addition to its effects on endothelial function, magnesium influences heart remodelling processes. It helps regulate the balance between cardiac muscle contraction and relaxation, critical for maintaining optimal heart function, particularly for those at risk of developing heart failure. [8]
Anti-inflammatory Effects
Magnesium exhibits anti-inflammatory properties, which are beneficial for heart health. Chronic inflammation is a crucial driver of cardiovascular diseases, including atherosclerosis and coronary artery disease. By reducing inflammation, magnesium helps protect the heart and blood vessels from damage and dysfunction, lowering the risk of cardiovascular events and reducing your risk of diabetes. [9-11]
Cardiovascular Risk Reduction
Combining all these effects, we know adequate magnesium intake significantly improves outcomes. By supporting endothelial function, preventing adverse heart remodeling, and exerting anti-inflammatory effects, adequate blood magnesium levels reduce cardiovascular risk and promote heart health.
Magnesium – where to find it?
Now, this is all well and good, but that begs the question – how do I keep my magnesium intake up?
Luckily, magnesium is present in many readily available food staples, namely nuts, brown rice, and even some cereals and bread! Whether you integrate this into your daily meals or look to nuts like almonds or cashews for a quick snack when peckish, maintaining your daily intake is not at all difficult!
Making some of the food items available or tweaking your diet slightly (for example, using wholegrain bread or brown rice) will quickly help you keep your levels adequate.
| Food | Milligrams (mg) per serving | Percent Daily intake* |
| Pumpkin seeds, roasted, 30g | 156 | 37 |
| Chia seeds, 30g | 111 | 26 |
| Almonds, dry roasted, 30g | 80 | 19 |
| Spinach, boiled, ½ cup | 78 | 19 |
| Cashews, dry roasted, 30g | 74 | 18 |
| Peanuts, oil roasted, ¼ cup | 63 | 15 |
| Cereal, shredded wheat, 2 large biscuits | 61 | 15 |
| Soymilk, plain or vanilla, 1 cup | 61 | 15 |
| Edamame, shelled, cooked, ½ cup | 50 | 12 |
| Potato, baked with skin, 100g | 43 | 10 |
| Rice, brown, cooked, ½ cup | 42 | 10 |
| Yogurt, plain, low fat, 225g | 42 | 10 |
| Breakfast cereals, fortified with 10% of the DV for magnesium, 1 serving | 42 | 10 |
| Oatmeal, instant, 1 packet | 36 | 9 |
| Kidney beans, canned, ½ cup | 35 | 8 |
| Banana, 1 medium | 32 | 8 |
| Salmon, Atlantic, farmed, cooked, 100g | 30 | 7 |
| Milk, 1 cup | 24 | 6 |
| Bread, whole wheat, 1 slice | 23 | 5 |
| Avocado, ½ cup | 22 | 5 |
| Chicken breast, roasted, 100g | 25 | 6 |
| Beef, ground, 90% lean, pan broiled, 100g | 23 | 5 |
| Broccoli, chopped and cooked, ½ cup | 12 | 3 |
| Rice, white, cooked, ½ cup | 10 | 2 |
| Apple, 1 medium | 9 | 2 |
| Carrot, raw, 1 medium | 7 | 2 |
Table 1. Some common magnesium-rich foods. Data sourced from: NIH – Office of Dietary Supplements.
For inspiration, see our simple and delicious salmon dish, which incorporates a few of those magnesium-rich foods.
Finally, keeping your magnesium levels within the “normal” range is important, as excess supplementation can lead to adverse effects, such as diarrhea and dangerous heart rhythms. Always consult with your healthcare professional.
Some medications, particularly diuretics (or medications used to treat acid reflux, such as proton pump inhibitors or PPIs), can disrupt normal magnesium homeostasis for those with heart failure or other conditions requiring medications. As such, some of us need just a little bit extra to keep our levels sufficient—always discuss oral magnesium supplementation and your requirements with your healthcare professional.
Conclusion
Hopefully, this whirlwind trip around magnesium homeostasis has enhanced your knowledge of this powerful little mineral and why ensuring adequate oral magnesium intake is so important. From better sleep to improved cardiovascular outcomes, magnesium is one of the quiet workhorses of the human body.
Keep an eye out for our upcoming review on different magnesium supplements, and be sure to subscribe to our newsletter to stay updated!
References
- Zhang Y, Chen C, Lu L, Knutson KL, Carnethon MR, Fly AD, et al. Association of magnesium intake with sleep duration and sleep quality: findings from the CARDIA study. Sleep. 2022;45(4).
- Reno AM, Green M, Killen LG, O’Neal EK, Pritchett K, Hanson Z. Effects of Magnesium Supplementation on Muscle Soreness and Performance. J Strength Cond Res. 2022;36(8):2198-203.
- Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24(2):47-66.
- Khan AM, Lubitz SA, Sullivan LM, Sun JX, Levy D, Vasan RS, et al. Low serum magnesium and the development of atrial fibrillation in the community: the Framingham Heart Study. Circulation. 2013;127(1):33-8.
- Pati G, Mukherjee S, Kumar P, Khan D, Sengupta S. A study of the effects of intravenous magnesium sulphate on post-operative atrial fibrillation in patients undergoing off pump coronary artery bypass grafting (CABG). Indian Journal of Clinical Anaesthesia. 2023;10(1):26-31.
- Parsanathan R. Trace element magnesium: a key player in hypertension management. Hypertension Research. 2023;46(10):2442-4.
- Shechter M, Sharir M, Labrador MJP, Forrester J, Silver B, Bairey Merz CN. Oral magnesium therapy improves endothelial function in patients with coronary artery disease. Circulation. 2000;102(19):2353-8.
- Tangvoraphonkchai K, Davenport A. Magnesium and Cardiovascular Disease. Adv Chronic Kidney Dis. 2018;25(3):251-60.
- Ashique S, Kumar S, Hussain A, Mishra N, Garg A, Gowda BHJ, et al. A narrative review on the role of magnesium in immune regulation, inflammation, infectious diseases, and cancer. J Health Popul Nutr. 2023;42(1):74.
- Nielsen FH. Magnesium deficiency and increased inflammation: current perspectives. J Inflamm Res. 2018;11:25-34.
- Rosique-Esteban N, Guasch-Ferré M, Hernández-Alonso P, Salas-Salvadó J. Dietary Magnesium and Cardiovascular Disease: A Review with Emphasis in Epidemiological Studies. Nutrients. 2018;10(2).