In the medical field, pacemakers have made notable changes in treating cardiac conditions. These small electronic devices have played an important role in aiding many people across the globe to maintain a steady and healthy heartbeat. From their early origins to modern advancements, pacemakers have become a significant option for managing heart rhythm disorders. This article will explore pacemakers’ history, functions, types, and impact on patients’ lives.
The Evolution of Pacemakers
The first pacemaker, developed in the late 1950s, was a bulky external device that required the patient to be plugged into an electrical outlet. Since then, technological advancements have transformed pacemakers into compact, implantable devices. Today’s pacemakers are intricately designed and offer a range of features that cater to the specific needs of patients.

Pacemakers, designed to regulate heart rhythm, exhibit variations in their physical appearances. This assortment includes different forms, from compact and discreet designs to slightly larger models. The variability in pacemaker size and shape allows for personalized treatment options based on patient needs and medical requirements.
Understanding How Pacemakers Work
Pacemakers are primarily used to regulate slow and abnormal heart rhythms, known as arrhythmias. These devices have two main components: the pulse generator and the leads. The pulse generator, which houses the battery and the electronic circuitry, is implanted under the skin, usually in the chest area. The leads, thin insulated wires, are threaded through a vein and connected to the heart.
The pacemaker continuously monitors the heart’s electrical activity. When it detects an abnormal rhythm or a pause in the heartbeat, it sends electrical impulses through the leads to stimulate the heart muscles and restore a regular rhythm. This process ensures the heart maintains an optimal rate and rhythm, improving the patient’s overall well-being.
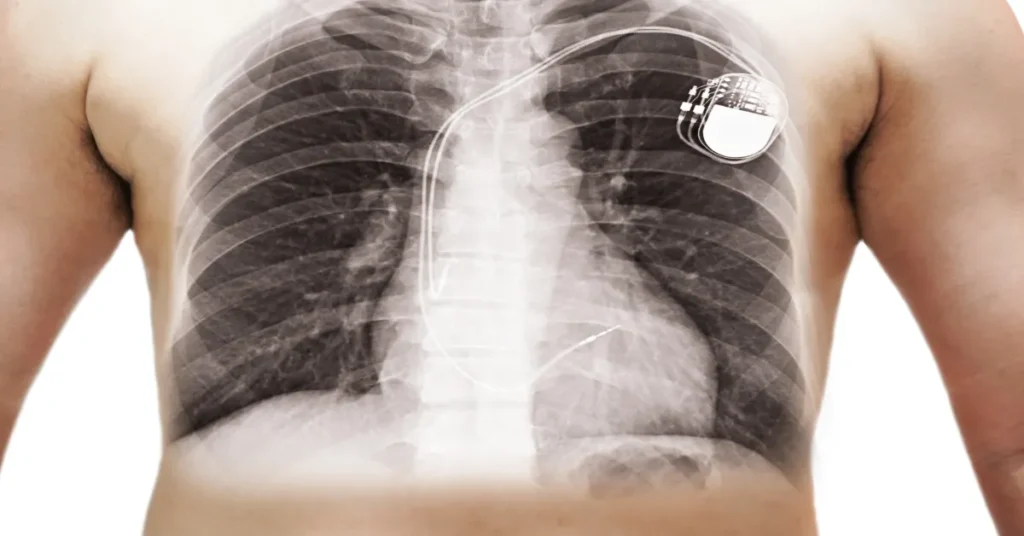
An X-ray overlay of the chest demonstrates the pacemaker’s typical position. If you are right-handed, the pacemaker is placed under the left collarbone bone to allow you to use your dominant hand unrestrictedly while you recover from the procedure. Leads are then passed via one of the veins that drain into the right side of the heart.
Types of Pacemakers:
- Single-Chamber Pacemakers: These pacemakers have one lead on the right side of the heart. They are primarily used to treat specific types of heart block or for patients with slow heart rates and atrial fibrillation (irregular heartbeat).
- Dual-Chamber Pacemakers: Dual-chamber pacemakers have two leads, one placed in the atrium and the other in the ventricle. They can coordinate the timing between the atria and ventricles, allowing for a more natural and synchronized heartbeat.
- Biventricular Pacemakers: Also known as cardiac resynchronization therapy (CRT) devices, biventricular pacemakers are designed for patients with heart failure and ventricular dyssynchrony, which occurs when the right and left sides of the heart are not working in sync. This causes heart muscle weakening and symptoms. These devices stimulate both ventricles simultaneously, improving the heart’s pumping efficiency.
- Leadless pacemakers—these innovative devices perform a similar function to conventional pacemakers, causing electrical stimulation of the heart. However, they do not require a lead and are directly implanted into the muscle of the right side of the heart via the femoral vein (in the groin region). Recently, there have been reports of further technological innovations, which you can read here.
Advancements in Pacemaker Technology
Over the years, pacemaker technology has undergone significant advancements. Modern pacemakers now come equipped with rate-responsive pacing, which adjusts the heart rate based on the patient’s physical activity levels. They can also collect and transmit data wirelessly, allowing healthcare providers to monitor the patient’s heart rhythm and device performance remotely.
Another notable advancement is the development of leadless pacemakers, self-contained units implanted directly into the heart without needing leads. These leadless pacemakers reduce the risk of lead-related complications and provide a less invasive option for patients.

Benefits of Pacemaker Implantation
Pacemaker implantation can provide several benefits, including:
-
Improved quality of life: Pacemakers can relieve symptoms such as fatigue, dizziness, and fainting, significantly improving a person’s quality of life.
-
Prevent complications: Pacemakers can prevent heart failure, stroke, and sudden cardiac arrest by maintaining a steady heartbeat.
-
Increased longevity: Pacemakers can increase life expectancy by preventing complications and improving heart function. One of the more devastating complications of a slow pulse rate is fainting or syncope, which can lead to falls and subsequent bone fractures. Unfortunately, this scenario is commonly observed in older populations, who are at a higher risk of sustaining life-changing injuries, including head trauma and fractures in the hip and leg bones.
Risks of Pacemaker Implantation
While pacemaker implantation is generally considered safe, there are some risks associated with the procedure, including:
- Infection: There is a risk of infection at the pacemaker implantation site, which can lead to complications.
- Bleeding or bruising: The implantation site may bleed or bruise, especially if the person takes blood-thinning medications.
- Damage to the heart or blood vessels: There is a risk of damage to the heart or blood vessels during the procedure, which can lead to serious complications.
- Lead displacement or malfunction: There is a risk of lead displacement or malfunction, which can lead to a loss of pacing or irregular heartbeats.
Living with a Pacemaker
Life can essentially return to normal for individuals with pacemakers. Many activities, including exercise, travel, and recreational pursuits, can be resumed with proper care and follow-up appointments. Although certain precautions need to be taken, such as avoiding electromagnetic solid fields or undergoing specific medical procedures, pacemaker recipients can enjoy an improved quality of life with the peace of mind that their heart rhythm is constantly monitored and regulated.
How long does the pacemaker battery last?
A common question among individuals with pacemakers is, “How long will the pacemaker battery last?” The lifespan of a pacemaker battery varies depending on several factors, including the type of device, the settings programmed, and the patient’s usage. On average, pacemaker batteries typically last between 5 to 15 years. However, advancements in battery technology have led to longer-lasting batteries in recent years. It is important to note that when the battery nears the end of its life, the pacemaker will need to be replaced, or the battery can be replaced during a routine surgical procedure. Regular follow-up appointments with a cardiologist or electrophysiologist are essential to monitor the battery life and ensure timely battery replacement when necessary, ensuring the pacemaker continues to function optimally and provides the necessary support for the patient’s heart rhythm.
Pacemaker FAQ
Q1: Can I fly if I have a pacemaker? A1: Yes, it is generally safe to fly with a pacemaker. However, it is recommended that you inform the airport security staff about your pacemaker, as it might trigger the metal detector. The electromagnetic environment on an airplane is unlikely to interfere with your pacemaker’s function.
Q2: Can I use a microwave if I have a pacemaker? A2: Yes, using a microwave is generally safe for individuals with pacemakers. Microwaves produce non-ionizing radiation, which is not known to interfere with pacemaker function. Still, maintaining a safe distance and avoiding prolonged exposure is advisable.
Q3: Can I have an MRI scan with a pacemaker? A3: While some modern pacemakers are designed to be MRI-compatible, many older models are not. Discussing your pacemaker with your healthcare provider is crucial if you need an MRI. CT scans can be an alternative testing method, utilizing radiation instead of magnetic fields, thereby not affecting your pacemaker. They can determine if your pacemaker is MRI-safe and, if not, suggest alternatives or precautions to ensure your safety.
Q4: Can I use an induction hot plate in the kitchen if I have a pacemaker? A4: Induction hot plates generate electromagnetic fields that may interfere with the function of pacemakers. While they are generally considered safe for individuals with pacemakers, it’s recommended to maintain a reasonable distance (e.g., 60cm/2 ft) from the hot plate while it’s in operation. Most people should be able to use a hob if they follow these precautions, but if you are choosing a new cooker, it may be easier to pick one that is not an induction hob. If you have any concerns, consult your healthcare provider for personalized guidance on using induction appliances safely with a pacemaker.
It is crucial to consult with a healthcare professional and follow their advice regarding specific activities and precautions to ensure the pacemaker’s optimal performance and personal well-being.
Conclusion
Pacemakers are an effective treatment option for people with arrhythmias or heart failure. They regulate the heartbeat through electrical impulses, which can improve quality of life, prevent complications, and increase longevity. While some risks are associated with pacemaker implantation, these are generally considered low, and the benefits typically outweigh the risks. If you’re considering a pacemaker, it’s important to discuss the procedure and its risks and benefits with your doctor to determine if it’s the right treatment option.
Heart Matters, edited by cardiologist Professor Peter Barlis, is a trusted resource that offers clear and accurate information on cardiovascular health. It bridges the gap between scientific research and everyday understanding, empowering you to make informed choices and take an active role in supporting your heart health.









