Upon receiving a prescription for a new medication called Entresto from your cardiologist, you may be curious to learn more about it. In this article, we’ll delve into the key aspects of Entresto, offering insights to help you understand its role in managing heart conditions effectively.
Entresto (sacubitril/valsartan) is a medication developed to address heart failure, a relatively common condition in our community that occurs when the heart’s pumping ability falls below optimal levels. This can result in various symptoms, including shortness of breath, fatigue, dizziness, leg swelling, and difficulty performing everyday activities. Combining sacubitril and valsartan, Entresto provides an effective solution, especially when initial treatments involving medications like ACE inhibitors and angiotensin receptor blockers (ARBs) prove inadequate. By enhancing cardiac function, this dual-action medication alleviates symptoms and reduces the risk of hospitalization and adverse outcomes associated with heart failure.
What is heart failure?
Heart failure, a complex and chronic condition, occurs when the heart struggles to pump blood effectively, leading to insufficient oxygen and nutrients to the body’s tissues. It often develops as a result of underlying health issues such as coronary artery disease, high blood pressure, or heart valve disorders. There are two main types of heart failure: systolic and diastolic.
Systolic heart failure, or heart failure with reduced ejection fraction (HFrEF), happens when the heart’s pumping ability weakens, causing reduced ejection fraction or the amount of blood pumped out with each heartbeat.
Diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF), occurs when the heart’s muscular walls become stiff and less able to relax during the filling phase, leading to impaired blood flow.
Both types present with similar symptoms like fatigue, shortness of breath, and fluid retention, yet they require tailored approaches to management. Consulting a healthcare provider for an accurate diagnosis and appropriate treatment strategy is essential in effectively addressing heart failure and its specific type.
General Principles of Heart Failure Management
Heart failure management follows a comprehensive approach to improve patients’ quality of life and reduce hospitalizations. Lifestyle modifications play a pivotal role, including maintaining a heart-healthy diet low in sodium and saturated fats, managing fluid intake, and engaging in regular physical activity as tolerated.
Medication adherence is crucial, with treatments like ACE inhibitors, beta-blockers, and diuretics commonly prescribed to optimize heart function and alleviate symptoms. Monitoring weight fluctuations and recognizing signs of worsening symptoms are vital to prevent exacerbations.
Collaborating closely with healthcare professionals to fine-tune treatment plans, attending regular follow-up appointments, and staying informed about heart failure can empower individuals to manage their condition and lead more fulfilling lives actively.
What is Entresto (sacubutril/valsartan)
Entresto (sacubitril/valsartan) is a medication specifically designed to treat heart failure. It combines two types of medicines: sacubitril and valsartan. Sacubitril is an inhibitor of neprilysin (an enzyme that breaks down certain hormones), while valsartan is an angiotensin receptor blocker (ARB) often used to treat high blood pressure and, on its own, as an initial treatment for heart failure.
The active components of Entresto, sacubitril, and valsartan function in distinct ways. Sacubitril inhibits the breakdown of natriuretic peptides, reducing strain on the heart by promoting sodium and water excretion in the urine. This action also decreases blood pressure and safeguards the heart from developing fibrosis—scar tissue that arises in heart failure. Valsartan, an ‘angiotensin-II-receptor antagonist,’ hinders the effects of an angiotensin II hormone. By blocking the receptors where angiotensin II usually attaches, valsartan prevents the hormone’s harmful effects on the heart and facilitates blood vessel dilation, thus reducing blood pressure.
Entresto dosing and administration
Entresto is available in three strengths: 24/26 mg, 49/51 mg, and 97/103 mg, which signify the sacubitril and valsartan content in each tablet. This medication is often considered after initial therapies with ACE inhibitors (ACEIs) fail to address heart failure, and ARBs prove inadequate.
Importantly, Entresto should not be combined with ACE inhibitors, as there must be a washout period before transitioning from an ACE inhibitor to Entresto. This precaution is essential to avoid the risk of increased angioedema—a rare but serious side effect. Your healthcare provider will guide you through the transition process to ensure your safety and effective management of your heart condition.
Entresto is taken twice a day as tablets. Like many medications, the treatment typically commences with a lower dosage to ensure effectiveness and comfort. Over a few weeks, the dosage can be gradually increased while closely observing how your body responds, any symptoms you may experience, your blood pressure levels, and the results of blood tests assessing kidney function. This cautious approach ensures the medication suits you well and achieves the desired outcomes.
Evidence for Entresto in heart failure
In a primary study, Entresto demonstrated its effectiveness in treating heart failure among adults. This study involved comparing Entresto and enalapril, another medication used for heart failure. The participants in the study had long-standing heart failure accompanied by symptoms of the condition and reduced ejection fraction (the portion of blood leaving the heart). Among those treated with Entresto, 21.8% (914 out of 4,187) of patients either experienced heart and circulation-related complications or were hospitalized due to heart failure. In contrast, 26.5% (1,117 out of 4,212) of patients treated with enalapril faced similar issues. The study spanned approximately 27 months, during which the participants took the medication for an average of around 24 months. The study was concluded prematurely due to compelling evidence indicating that Entresto was more effective than enalapril in these aspects.
| Sacubitril/valsartan 97/103 mg twice daily | Enalapril 10 mg twice daily | |
| Composite primary outcome: death from cardiovascular causes or hospitalization from worsening heart failure | 21.8% (914/4187) | 26.5% (1117/4212) |
| Death from cardiovascular causes | 13.3% (558/4187) | 16.5% (693/4212) |
| Hospitalization from worsening heart failure | 12.8% (537/4187) | 15.6% (658/4212) |
Table – Efficacy of sacubitril/valsartan compared to enalapril in chronic heart failure. The PARADIGM-HF trial (Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure) was a landmark clinical trial that brought significant insights into heart failure management. This trial compared the effects of a novel medication, Entresto (sacubitril/valsartan), with the traditional ACE inhibitor enalapril in patients with heart failure and reduced ejection fraction (HFrEF).
The trial’s results demonstrated that Entresto was more effective than enalapril in reducing the risk of cardiovascular death and hospitalization due to heart failure. This pivotal finding led to the early termination of the study, highlighting the clear advantage of Entresto over the standard ACE inhibitor treatment.
Side effects and precautions
Entresto has specific considerations and potential side effects to be aware of:
- Contraindication with ACE Inhibitors: Entresto is contraindicated when used concurrently with ACE inhibitors. It’s important not to administer entresto within 36 hours of switching between entresto and an ACE inhibitor. Additionally, it should not be used in combination with aliskiren in patients with diabetes.
- Angioedema Awareness: Entresto can cause angioedema, a serious condition characterized by localized swelling, including the larynx. If you have hereditary angioedema, it’s best to avoid Entresto.
- Low blood pressure (Hypotension) Awareness: Entresto may lead to lower blood pressure, potentially causing symptoms of low blood pressure (hypotension). Patients with activated renin-angiotensin systems, particularly those with reduced fluid or salt levels, may be more vulnerable. To address this, ensure proper fluid and salt balance before starting Entresto or consider commencing with a lower dose. If low blood pressure symptoms persist despite adjustments, dose reduction or temporary pause might be considered. Usually, permanent discontinuation is not required.
- Impaired Renal Function: Entresto may decrease renal function, particularly in susceptible individuals. Regular blood tests should be used to monitor kidney function closely for patients whose renal function depends on the renin-angiotensin-aldosterone system.
- Hyperkalemia (high potassium level): Entresto can cause hyperkalemia (high potassium levels). Monitor serum potassium regularly, especially in patients at risk for hyperkalemia, and treat accordingly.
- Interactions and Precautions: Avoid concurrent use of potassium-sparing diuretics, potassium supplements, or salt substitutes containing potassium, as these can increase serum potassium levels. Avoid entresto with angiotensin II receptor blockers (ARBs) due to the presence of valsartan. When taking lithium, monitor serum lithium levels during concurrent use with entresto.
It’s crucial to be aware of these potential effects and follow your healthcare provider’s guidance when considering or using Entresto. For a comprehensive understanding of side effects, please refer to the package leaflet or consult your doctor or pharmacist.

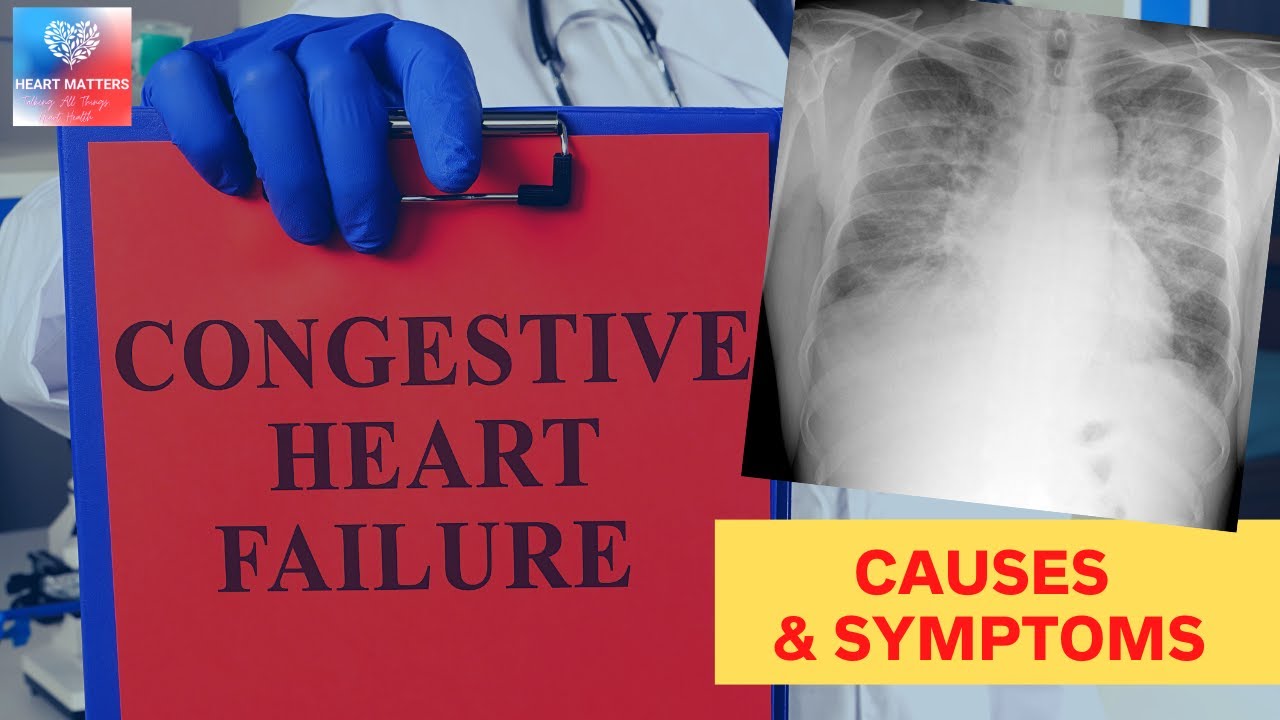
This figure illustrates a chest X-ray (CXR) showcasing characteristic heart failure-associated pulmonary edema findings. The CXR exhibits prominent bilateral opacities in the lung fields, resembling bat wings. These opacities indicate fluid accumulation within the lung tissues, a hallmark of congestive heart failure. The bat wings’ appearance results from fluid overload, which causes increased interstitial and alveolar fluid, leading to widespread haziness in the lung fields.

Conclusion
In summary, Entresto (sacubitril/valsartan) significantly advances heart failure treatment. This medication combines sacubitril and valsartan to effectively address heart failure complexities, enhancing cardiac function, easing symptoms, and reducing hospitalization risks. Supported by robust clinical evidence, Entresto exemplifies medical progress, offering a pragmatic approach to improving the well-being and longevity of individuals grappling with heart failure. Heart failure management remains multifaceted, underscoring the importance of lifestyle monitoring such as regular weight checks and medication adherence. Your healthcare provider can offer tailored guidance on integrating Entresto into your heart health strategy.